We hoorden het de afgelopen tijd regelmatig. “Er is geen bewijs” voor: mondkapjes, aerosolen, 1,5 meter, vitamine D, hydroxychloroquine, verspreiding door kinderen, etc.1 We hebben te maken met het ‘argument van onwetendheid’. Daarbij wordt aangenomen dat een stelling onwaar is, omdat niet bewezen is dat deze waar is. Of, omgekeerd, dat deze waar is, omdat niet bewezen is dat het gestelde onwaar is.2 Soms is het onderwerp niet eens onderzocht, nog afgezien van het gehanteerde criterium voor ‘bewijs’. Bovendien is ‘een feit’ niet afhankelijk van het vermogen van de mens om een feit te kunnen vaststellen. Dikwijls kan het ultieme bewijs niet worden geleverd. Medisch-ethische toetsingscommissies zitten niet te wachten op het blootstellen van gezonde mensen aan aerosolen met SARS-CoV-2.
Beste bezoeker, u heeft geen toegang.
Enkel (web)abonnees hebben toegang tot tijdschriftartikelen. Het webabonnement is nog in de maak.
U kunt zich wel alvast (gratis) registreren en tal van andere webartikelen raadplegen!
Auteur
Trefwoorden:
Verschenen in
Referenties
1. Een korte versie verscheen op 30 juli 2020 in de online uitgave van “Medisch Contact”.
Muskiet FAJ. Covid-19 en het ‘argument van de onwetendheid’.
https://www.medischcontact.nl/opinie/reacties/ingezonden-reactie/covid-1...'argument%20van%20de%20onwetendheid',-Plaats%20een%20reactie&text='Er%20is%20geen%20bewijs'%20voor,is%20dat%20het%20waar%20is.
2. Wikipedia. Argumentum ad ignorantiam of het argument van de onwetendheid.
https://nl.wikipedia.org/wiki/Argumentum_ad_ignorantiam#:~:text=Argument....
3. In Voedingsgeneeskunde werd reeds eerder aandacht besteed aan “Evidence Based Medicine”.
Muskiet FA. Wat is ’bewijs’ in de gezondheidszorg en voedingswetenschap? Voedingsgeneeskunde 2017;18(4):32-35.
https://www.voedingsgeneeskunde.nl/vg-18-4/wat-bewijs-de-gezondheidszorg...
4. Wikipedia. Falsifieerbaarheid.
https://nl.wikipedia.org/wiki/Falsifieerbaarheid
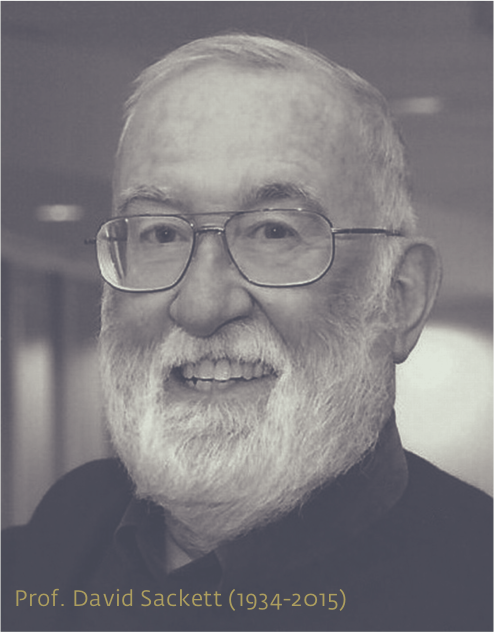
5. Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312(7023):71-72. doi:10.1136/bmj.312.7023.71
https://pubmed.ncbi.nlm.nih.gov/8555924/
6. Sackett DL. Evidence-based medicine. Semin Perinatol. 1997;21(1):3-5. doi:10.1016/s0146-0005(97)80013-4
https://pubmed.ncbi.nlm.nih.gov/9190027/
7. Sackett DL, Strauss SE, Richardson WS, Rosenberg W, Haynes RB. Evidence-Based Medicine: How to Practice and Teach EBM. Churchill Livingstone (second edition, Feb. 2000). ISBN 0443062404.
https://www.worldcat.org/title/evidence-based-medicine-how-to-practice-a...
8. Jamilloux Y, Henry T, Belot A, et al. Should we stimulate or suppress immune responses in COVID-19? Cytokine and anti-cytokine interventions. Autoimmun Rev. 2020;19(7):102567. doi:10.1016/j.autrev.2020.102567
https://pubmed.ncbi.nlm.nih.gov/32376392/
9. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China [published correction appears in Lancet. 2020 Jan 30;:]. Lancet. 2020;395(10223):497-506. doi:10.1016/S0140-6736(20)30183-5
https://pubmed.ncbi.nlm.nih.gov/31986264/
10. Cole SA, Laviada-Molina HA, Serres-Perales JM, Rodriguez-Ayala E, Bastarrachea RA. The COVID-19 Pandemic during the Time of the Diabetes Pandemic: Likely Fraternal Twins?. Pathogens. 2020;9(5):389. Published 2020 May 19. doi:10.3390/pathogens9050389
https://pubmed.ncbi.nlm.nih.gov/32438687/
11. Pedersen SF, Ho YC. SARS-CoV-2: a storm is raging. J Clin Invest. 2020;130(5):2202-2205. doi:10.1172/JCI137647
https://pubmed.ncbi.nlm.nih.gov/32217834/
12. Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome [published correction appears in Lancet Respir Med. 2020 Feb 25;:]. Lancet Respir Med. 2020;8(4):420-422. doi:10.1016/S2213-2600(20)30076-X
https://pubmed.ncbi.nlm.nih.gov/32085846/
13. McGonagle D, O'Donnell JS, Sharif H, Emery P, Bridgewood C. Immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia. Lancet Rheumatology VOLUME 2, ISSUE 7, E437-E445, JULY 01, 2020. Published: May 07, 2020, DOI: https://doi.org/10.1016/S2665-9913(20)30121-1
https://www.thelancet.com/journals/lanrhe/article/PIIS2665-9913(20)30121-1/fulltext
14. Tisoncik JR, Korth MJ, Simmons CP, Farrar J, Martin TR, Katze MG. Into the eye of the cytokine storm. Microbiol Mol Biol Rev. 2012;76(1):16–32. doi:10.1128/MMBR.05015-11
https://pubmed.ncbi.nlm.nih.gov/22390970/?from_single_result=Tisoncik%2C...
15. Canna SW, Behrens EM. Making sense of the cytokine storm: a conceptual framework for understanding, diagnosing, and treating hemophagocytic syndromes. Pediatr Clin North Am. 2012;59(2):329–344. doi:10.1016/j.pcl.2012.03.002
https://pubmed.ncbi.nlm.nih.gov/22560573/?from_single_result=Canna+Pedia...
16. Teijaro JR, Walsh KB, Rice S, Rosen H, Oldstone MB. Mapping the innate signaling cascade essential for cytokine storm during influenza virus infection. Proc Natl Acad Sci U S A. 2014;111(10):3799–3804. doi:10.1073/pnas.1400593111
https://pubmed.ncbi.nlm.nih.gov/24572573/?from_single_result=Mapping+the...
17. Liu Q, Zhou YH, Yang ZQ. The cytokine storm of severe influenza and development of immunomodulatory therapy. Cell Mol Immunol. 2016;13(1):3–10. doi:10.1038/cmi.2015.74
https://pubmed.ncbi.nlm.nih.gov/26189369/?from_term=The+cytokine+storm+i...
18. Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017;39(5):529–539. doi:10.1007/s00281-017-0629-x
https://pubmed.ncbi.nlm.nih.gov/28466096/?from_single_result=Channappana...
19. Shimabukuro-Vornhagen A, Gödel P, Subklewe M, et al. Cytokine release syndrome. J Immunother Cancer. 2018;6(1):56. Published 2018 Jun 15. doi:10.1186/s40425-018-0343-9
https://pubmed.ncbi.nlm.nih.gov/29907163/?from_single_result=Shimabukuro...
20. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China [published online ahead of print, 2020 Mar 3]. Intensive Care Med. 2020;1–3. doi:10.1007/s00134-020-05991-x
https://pubmed.ncbi.nlm.nih.gov/32125452/?from_single_result=Ruan+Intens...
21. Cron R, Chatham W. How doctors can potentially significantly reduce the number of deaths from Covid-19. We already have medicines for treating cytokine storm syndrome, the immune response that’s killing many who die of Covid-19
https://www.vox.com/2020/3/12/21176783/coronavirus-covid-19-deaths-china...
22. Sarzi-Puttini P, Giorgi V, Sirotti S, et al. COVID-19, cytokines and immunosuppression: what can we learn from severe acute respiratory syndrome?. Clin Exp Rheumatol. 2020;38(2):337–342.
https://pubmed.ncbi.nlm.nih.gov/32202240/?from_term=Sarzi-Puttini+Clin+E...
23. Cusabo. What You Have to Know about Cytokine Storm and Virus Infection. Accessed 30/07/20.
https://www.cusabio.com/c-20981.html
24. Argyropoulos KV, Serrano A, Hu J, et al. Association of Initial Viral Load in Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Patients with Outcome and Symptoms [published online ahead of print, 2020 Jul 3]. Am J Pathol. 2020;S0002-9440(20)30328-X.
https://pubmed.ncbi.nlm.nih.gov/32628931/
25. McNamara D. Unexpected: Higher Viral Loads Seen in Less Severe COVID-19. Medscape - Jul 17, 2020.
https://www.medscape.com/viewarticle/934147
26. Wang Q, Fang P, He R, et al. O-GlcNAc transferase promotes influenza A virus-induced cytokine storm by targeting interferon regulatory factor-5. Sci Adv. 2020;6(16):eaaz7086. Published 2020 Apr 15. doi:10.1126/sciadv.aaz7086.
https://pubmed.ncbi.nlm.nih.gov/32494619/
27. Williams R. Discovered: Metabolic Mechanism of Cytokine Storms. The Scientist, accessed 30/7/2020.
https://www.the-scientist.com/news-opinion/discovered-metabolic-mechanis...
28. Frates EP, Rifai T. Making the Case for "COVID-19 Prophylaxis" With Lifestyle Medicine. Am J Health Promot. 2020;34(6):689-691. doi:10.1177/0890117120930536c
https://pubmed.ncbi.nlm.nih.gov/32551935/
29. Stefan N, Birkenfeld AL, Schulze MB, Ludwig DS. Obesity and impaired metabolic health in patients with COVID-19. Nat Rev Endocrinol. 2020;16(7):341-342. doi:10.1038/s41574-020-0364-6
https://pubmed.ncbi.nlm.nih.gov/32327737/
30. Finer N, Garnett SP, Bruun JM. COVID-19 and obesity. Clin Obes. 2020;10(3):e12365. doi:10.1111/cob.12365
https://pubmed.ncbi.nlm.nih.gov/32342637/
31. Luzi L, Radaelli MG. Influenza and obesity: its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol. 2020;57(6):759-764. doi:10.1007/s00592-020-01522-8
https://pubmed.ncbi.nlm.nih.gov/32249357/
32. Ryan DH, Ravussin E, Heymsfield S. COVID 19 and the Patient with Obesity - The Editors Speak Out. Obesity (Silver Spring). 2020;28(5):847. doi:10.1002/oby.22808
https://pubmed.ncbi.nlm.nih.gov/32237212/
33. Dietz W, Santos-Burgoa C. Obesity and its Implications for COVID-19 Mortality. Obesity (Silver Spring). 2020;28(6):1005. doi:10.1002/oby.22818
https://pubmed.ncbi.nlm.nih.gov/32237206/
34. Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91-95. doi:10.1016/j.ijid.2020.03.017
https://pubmed.ncbi.nlm.nih.gov/32173574/
35. Bornstein SR, Dalan R, Hopkins D, Mingrone G, Boehm BO. Endocrine and metabolic link to coronavirus infection. Nat Rev Endocrinol. 2020;16(6):297-298. doi:10.1038/s41574-020-0353-9
https://pubmed.ncbi.nlm.nih.gov/32242089/
36. Reaven GM. The metabolic syndrome: requiescat in pace. Clin Chem. 2005;51(6):931-938. doi:10.1373/clinchem.2005.048611
https://pubmed.ncbi.nlm.nih.gov/15746300/
37. Reaven GM. The insulin resistance syndrome: definition and dietary approaches to treatment. Annu Rev Nutr. 2005;25:391-406. doi:10.1146/annurev.nutr.24.012003.132155
https://pubmed.ncbi.nlm.nih.gov/16011472/
38. Muskiet FAJ. De evolutionaire achtergrond, oorzaak en consequenties van chronische systemische lage graad ontsteking; betekenis voor de klinische chemie. Ned Tijdschr Klin Chem Labgeneesk 2011; 36: 199-214
https://www.nvkc.nl/sites/default/files/NTKC/Evolutionaireachtergrondchr...
39. Muskiet FA, Muskiet MH. Chronische systemische lagegraadontsteking. De opmaat voor het insulineresistentiesyndroom en sequelae. Arts Therapeut & Apotheker 2012;13:10-16.
https://www.voedingsgeneeskunde.nl/ata-13-1/chronische-systemische-lageg...
40. Paolisso G, Barbieri M, Rizzo MR, et al. Low insulin resistance and preserved beta-cell function contribute to human longevity but are not associated with TH-INS genes. Exp Gerontol. 2001;37(1):149-156. doi:10.1016/s0531-5565(01)00148-6
https://pubmed.ncbi.nlm.nih.gov/11738155/
41. Barbieri M, Gambardella A, Paolisso G, Varricchio M. Metabolic aspects of the extreme longevity. Exp Gerontol. 2008;43(2):74-78. doi:10.1016/j.exger.2007.06.003
https://pubmed.ncbi.nlm.nih.gov/17697759/
42. Wang S, Ma P, Zhang S, et al. Fasting blood glucose at admission is an independent predictor for 28-day mortality in patients with COVID-19 without previous diagnosis of diabetes: a multi-centre retrospective study [published online ahead of print, 2020 Jul 10]. Diabetologia. 2020;1-10. doi:10.1007/s00125-020-05209-1
https://pubmed.ncbi.nlm.nih.gov/32647915/
43. Tucker ME. Hyperglycemia Predicts COVID-19 Death Even Without Diabetes. Medscape 13 July 2020.
https://www.medscape.com/viewarticle/933787?nlid=136394_5404&src=wnl_dne...
44. Leviton A, Dammann O. Coagulation, inflammation, and the risk of neonatal white matter damage. Pediatr Res. 2004;55(4):541-545. doi:10.1203/01.PDR.0000121197.24154.82
https://pubmed.ncbi.nlm.nih.gov/14973176/
45. Esmon CT. The interactions between inflammation and coagulation. Br J Haematol. 2005;131(4):417-430. doi:10.1111/j.1365-2141.2005.05753.x
https://pubmed.ncbi.nlm.nih.gov/20083910/
46. Levi M, van der Poll T. Inflammation and coagulation. Crit Care Med. 2010;38(2 Suppl):S26-S34. doi:10.1097/CCM.0b013e3181c98d21
https://pubmed.ncbi.nlm.nih.gov/16281932/
47. Yang Y, Tang H. Aberrant coagulation causes a hyper-inflammatory response in severe influenza pneumonia. Cell Mol Immunol. 2016;13(4):432-442. doi:10.1038/cmi.2016.1
https://pubmed.ncbi.nlm.nih.gov/27041635/
48. Mosevoll KA, Johansen S, Wendelbo Ø, Nepstad I, Bruserud Ø, Reikvam H. Cytokines, Adhesion Molecules, and Matrix Metalloproteases as Predisposing, Diagnostic, and Prognostic Factors in Venous Thrombosis. Front Med (Lausanne). 2018;5:147. Published 2018 May 22. doi:10.3389/fmed.2018.00147
https://pubmed.ncbi.nlm.nih.gov/29872658/
49. Paar V, Wernly B, Zhou Z, et al. Anti-coagulation for COVID-19 treatment: both anti-thrombotic and anti-inflammatory? [published online ahead of print, 2020 Jul 6]. J Thromb Thrombolysis. 2020;1-6. doi:10.1007/s11239-020-02212-6
https://pubmed.ncbi.nlm.nih.gov/32632558/
50. Belen-Apak FB, Sarıalioğlu F. Pulmonary intravascular coagulation in COVID-19: possible pathogenesis and recommendations on anticoagulant/thrombolytic therapy [published online ahead of print, 2020 May 5]. J Thromb Thrombolysis. 2020;1-3. doi:10.1007/s11239-020-02129-0
https://pubmed.ncbi.nlm.nih.gov/32372336/
51. van Gorp EC, Suharti C, ten Cate H, et al. Review: infectious diseases and coagulation disorders. J Infect Dis. 1999;180(1):176-186. doi:10.1086/314829
https://pubmed.ncbi.nlm.nih.gov/10353876/
52. EVMS CRITICAL CARE COVID-19 MANAGEMENT PROTOCOL. Developed and updated by Paul Marik, MD Chief of Pulmonary and Critical Care Medicine Eastern Virginia Medical School, Norfolk, VA June 17th, 2020
https://www.evms.edu/media/evms_public/departments/internal_medicine/EVM...
53. Delvaeye M, Conway EM. Coagulation and innate immune responses: can we view them separately?. Blood. 2009;114(12):2367-2374. doi:10.1182/blood-2009-05-199208
https://pubmed.ncbi.nlm.nih.gov/19584396/
54. Loof TG, Mörgelin M, Johansson L, et al. Coagulation, an ancestral serine protease cascade, exerts a novel function in early immune defense. Blood. 2011;118(9):2589-2598. doi:10.1182/blood-2011-02-337568
https://pubmed.ncbi.nlm.nih.gov/21613262/
55. Fiusa MM, Carvalho-Filho MA, Annichino-Bizzacchi JM, De Paula EV. Causes and consequences of coagulation activation in sepsis: an evolutionary medicine perspective. BMC Med. 2015;13:105. Published 2015 May 6. doi:10.1186/s12916-015-0327-2
https://pubmed.ncbi.nlm.nih.gov/25943883/
56. Wichmann D, Sperhake JP, Lütgehetmann M, et al. Autopsy Findings and Venous Thromboembolism in Patients With COVID-19 [published online ahead of print, 2020 May 6]. Ann Intern Med. 2020;M20-2003. doi:10.7326/M20-2003
https://pubmed.ncbi.nlm.nih.gov/32374815/
57. Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy Brown J, Vander Heide RS. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med. 2020;8(7):681-686. doi:10.1016/S2213-2600(20)30243-5
https://pubmed.ncbi.nlm.nih.gov/32473124/
58. Worcester S. Is Protocol-Driven COVID-19 Ventilation Doing More Harm Than Good? Medscape Apr 06, 2020.
https://www.medscape.com/viewarticle/928236
59. Gattinoni L, Coppola S, Cressoni M, Busana M, Rossi S, Chiumello D. COVID-19 Does Not Lead to a "Typical" Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med. 2020;201(10):1299-1300. doi:10.1164/rccm.202003-0817LE
https://pubmed.ncbi.nlm.nih.gov/32228035/
60. Federatie Medische Specialisten. Leidraad Corticosteroïden in beloop van COVID-19 pneumonie-ARDS beeld. Versie dd. 24 juli, 2020, accessed 31/07/2020
https://www.demedischspecialist.nl/sites/default/files/Leidraad%20Cortic...
61. Nile SH, Nile A, Qiu J, Li L, Jia X, Kai G. COVID-19: Pathogenesis, cytokine storm and therapeutic potential of interferons. Cytokine Growth Factor Rev. 2020;53:66-70. doi:10.1016/j.cytogfr.2020.05.002
https://pubmed.ncbi.nlm.nih.gov/32418715/
62. Texas Doctor Reverses Coronavirus Symptoms In 100% Of Cases With Inexpensive Treatment.
https://www.naturalblaze.com/2020/07/texas-doctor-reverses-coronavirus-s...
63. Armitage LC, Brettell R. Inhaled corticosteroids: A rapid review of the evidence for treatment or prevention of COVID-19. The Centre for Evidence-Based Medicine, June 22, 2020.
https://www.cebm.net/covid-19/inhaled-corticosteroids-a-rapid-review-of-...
64. Wang Q, Hu Z. Successful recovery of severe COVID-19 with cytokine storm treating with extracorporeal blood purification. Int J Infect Dis. 2020;96:618-620. doi:10.1016/j.ijid.2020.05.065
https://pubmed.ncbi.nlm.nih.gov/32470601/
65. Atal S, Fatima Z. IL-6 Inhibitors in the Treatment of Serious COVID-19: A Promising Therapy? [published online ahead of print, 2020 Jun 13]. Pharmaceut Med. 2020;1-9. doi:10.1007/s40290-020-00342-z
https://pubmed.ncbi.nlm.nih.gov/32535732/
66. Catanzaro M, Fagiani F, Racchi M, Corsini E, Govoni S, Lanni C. Immune response in COVID-19: addressing a pharmacological challenge by targeting pathways triggered by SARS-CoV-2. Signal Transduct Target Ther. 2020;5(1):84. Published 2020 May 29. doi:10.1038/s41392-020-0191-1
https://pubmed.ncbi.nlm.nih.gov/32467561/
67. Abdin SM, Elgendy SM, Alyammahi SK, Alhamad DW, Omar HA. Tackling the cytokine storm in COVID-19, challenges and hopes [published online ahead of print, 2020 Jul 11]. Life Sci. 2020;257:118054. doi:10.1016/j.lfs.2020.118054
https://pubmed.ncbi.nlm.nih.gov/32663575/
68. Doheny K. Low-Dose Radiation Therapy May Help COVID-19 Patients/ Medscape June 18. 2020.
https://www.medscape.com/viewarticle/932583
69a. Hess CB, Buchwald ZS, Stokes W, Switchenko JM, Nasti TH, Weinberg BD, Steinberg JP, Goddette KD, Ahmed R, Curran WC, Khan MK. Low-Dose Whole-Lung Radiation for COVID-19 Pneumonia: Planned Day-7 Interim Analysis of a Registered Clinical Trial
https://www.medrxiv.org/content/10.1101/2020.06.03.20116988v1
69b. Mehta P, McAuley DF, Brown M, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033-1034. doi:10.1016/S0140-6736(20)30628-0
https://pubmed.ncbi.nlm.nih.gov/32192578/
70. MATH+ hospital treatment protocol for COVID-19 to control inflammation and excess clotting.
https://covid19criticalcare.com/wp-content/uploads/2020/07/FLCCC_Allianc...
71. Ye Q, Wang B, Mao J. The pathogenesis and treatment of the `Cytokine Storm' in COVID-19. J Infect. 2020;80(6):607-613. doi:10.1016/j.jinf.2020.03.037
https://pubmed.ncbi.nlm.nih.gov/32283152/
72. RECOVERY Collaborative Group 2020. Effect of dexamethasone in hospitalized patients with COVID-19—preliminary report. 22 Jun 2020 (preprint).
https://www.medrxiv.org/content/10.1101/2020.06.22.20137273v1.full.pdf.
73. Mahase E. Covid-19: Low dose steroid cuts death in ventilated patients by one third, trial finds. BMJ. 2020;369:m2422. Published 2020 Jun 16. doi:10.1136/bmj.m2422
https://pubmed.ncbi.nlm.nih.gov/32546467/
74. Mahase E. Covid-19: Demand for dexamethasone surges as RECOVERY trial publishes preprint. BMJ. 2020;369:m2512. Published 2020 Jun 23. doi:10.1136/bmj.m2512
https://pubmed.ncbi.nlm.nih.gov/32576548/
75. Johnson RM, Vinetz JM. Dexamethasone in the management of covid -19. BMJ. 2020;370:m2648. Published 2020 Jul 3. doi:10.1136/bmj.m2648
https://pubmed.ncbi.nlm.nih.gov/32620554/
76. Zha L, Li S, Pan L, et al. Corticosteroid treatment of patients with coronavirus disease 2019 (COVID-19). Med J Aust. 2020;212(9):416-420. doi:10.5694/mja2.50577
https://pubmed.ncbi.nlm.nih.gov/32266987/
77. INTERNATIONAL PULMONOLOGIST’S CONSENSUS ON COVID-19. Editors: Dr. Tinku Joseph (India), Dr. Mohammed Ashkan Moslehi (Iran), Diagnosis and treatment plan of novel coronavirus pneumonia (Version 7) [EB/OL]. (2020-03-04)[2020-03-05
https://www.unah.edu.hn/dmsdocument/9674-consenso-internacional-de-neumo...
78. WHO. Clinical management of COVID-19. Interim guidance 27 May 2020, accessed 29 07 2020
file:///C:/Users/Eigenaar/Downloads/WHO-2019-nCoV-clinical-2020.5-eng%20(1).pdf
79. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China [published correction appears in Lancet. 2020 Jan 30;:]. Lancet. 2020;395(10223):497-506. doi:10.1016/S0140-6736(20)30183-5
https://pubmed.ncbi.nlm.nih.gov/31986264/
80. Russell CD, Millar JE, Baillie JK. Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury. Lancet. 2020;395(10223):473-475. doi:10.1016/S0140-6736(20)30317-2
https://pubmed.ncbi.nlm.nih.gov/32043983/
81. Lansbury L, Rodrigo C, Leonardi-Bee J, Nguyen-Van-Tam J, Lim WS. Corticosteroids as adjunctive therapy in the treatment of influenza. Cochrane Database Syst Rev. 2019;2(2):CD010406. Published 2019 Feb 24. doi:10.1002/14651858.CD010406.pub3
https://pubmed.ncbi.nlm.nih.gov/30798570/
82. Barton LM, Duval EJ, Stroberg E, Ghosh S, Mukhopadhyay S. COVID-19 Autopsies, Oklahoma, USA. Am J Clin Pathol. 2020;153(6):725-733. doi:10.1093/ajcp/aqaa062
https://pubmed.ncbi.nlm.nih.gov/32275742/
83. Carsana L, Sonzogni A, Nasr A, et al. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study [published online ahead of print, 2020 Jun 8]. Lancet Infect Dis. 2020;S1473-3099(20)30434-5. doi:10.1016/S1473-3099(20)30434-5
https://pubmed.ncbi.nlm.nih.gov/32526193/
84. Rapkiewicz AV, Mai X, Carsons SE, Pittaluga S, Kleiner DE, Berger JS, Thomas S, Adler NM, Charytan DM, Gasmi B, Hochman JS, Reynolds HR. Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: A case series. EClinicalMedicine Published: June 2020. DOI:https://doi.org/10.1016/j.eclinm.2020.100434
https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(20)30178-4/fulltext
85. Edler C, Schröder AS, Aepfelbacher M, et al. Dying with SARS-CoV-2 infection-an autopsy study of the first consecutive 80 cases in Hamburg, Germany [published correction appears in Int J Legal Med. 2020 Jun 19;:]. Int J Legal Med. 2020;134(4):1275-1284. doi:10.1007/s00414-020-02317-w
https://pubmed.ncbi.nlm.nih.gov/32500199/
86. Segerstrom SC. Stress, Energy, and Immunity: An Ecological View. Curr Dir Psychol Sci. 2007;16(6):326-330. doi:10.1111/j.1467-8721.2007.00522.x
https://pubmed.ncbi.nlm.nih.gov/18645630/
87. Straub RH, Cutolo M, Buttgereit F, Pongratz G. Energy regulation and neuroendocrine-immune control in chronic inflammatory diseases. J Intern Med. 2010;267(6):543-560. doi:10.1111/j.1365-2796.2010.02218.x
https://pubmed.ncbi.nlm.nih.gov/20210843/
88. Calder PC, Carr AC, Gombart AF, Eggersdorfer M. Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections. Nutrients. 2020;12(4):1181. Published 2020 Apr 23. doi:10.3390/nu12041181
https://pubmed.ncbi.nlm.nih.gov/32340216/
89. Calder PC. Nutrition, immunity and COVID-19. BMJ Nutrition, Prevention & Health 2020;3:e000085. doi:10.1136/bmjnph-2020-000085
https://nutrition.bmj.com/content/bmjnph/3/1/74.full.pdf
90. Kashiouris MG, L'Heureux M, Cable CA, Fisher BJ, Leichtle SW, Fowler AA. The Emerging Role of Vitamin C as a Treatment for Sepsis. Nutrients. 2020;12(2):292. Published 2020 Jan 22. doi:10.3390/nu12020292
https://pubmed.ncbi.nlm.nih.gov/31978969/
91. Stessel B, Vanvuchelena C, Bruckersc L, Geebelena L, Callebauta I, Vandenbrandea J, Pellensa B, Van Tornout M, Orya J-P, Van Halem K, Messiaen P, Herbotse L, Ramaekers D, Duboisa J. Impact of implementation of an individualised thromboprophylaxis protocol in critically ill ICU patients with COVID-19: A longitudinal controlled before-after study. Thrombosis Research 194 (2020) 209–215, doi.org/10.1016/j.thromres.2020.07.038
https://www.thrombosisresearch.com/article/S0049-3848(20)30329-7/fulltext
92. Verschillende specialisten organisaties. Leidraad COVID-19 coagulopathie. Diagnostiek en tromboprofylaxe bij diepe veneuze trombose en Longembolie. Accessed 4 augustus 2020.
https://www.demedischspecialist.nl/sites/default/files/Leidraad%20COVID-...
93 Lindeberg S, Eliasson M, Lindahl B, Ahrén B. Low serum insulin in traditional Pacific Islanders--the Kitava Study. Metabolism. 1999;48(10):1216-1219. doi:10.1016/s0026-0495(99)90258-5
https://pubmed.ncbi.nlm.nih.gov/10535381/