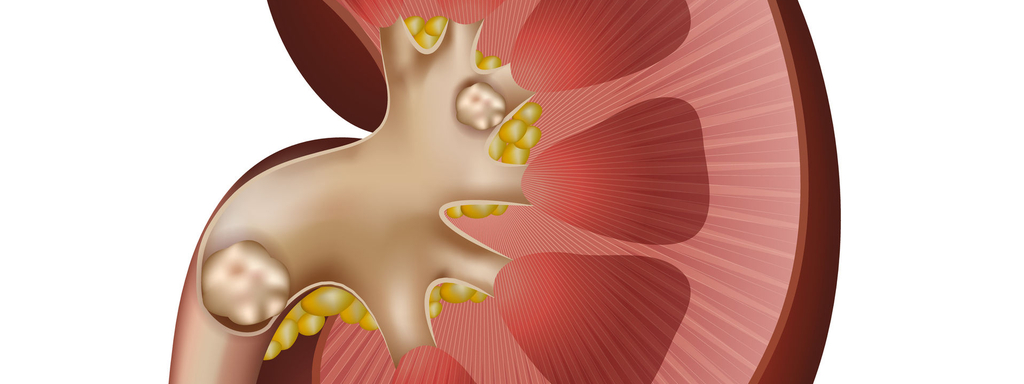
Nierstenen zijn een beschavingsziekte. Ze zijn een gevolg van slechte voeding, dus we kunnen ze oplossen met gezonde voeding. De scheikundige ('levenloze') pijlers van nierstenen zijn mineraalbalans (calcium, magnesium en kalium), oxalaat, citraat en zuurgraad. Deze pijlers hebben een duidelijke link met voeding: mits aanpassing van het voedingspatroon kunnen afwijkingen in de urinaire scheikunde gecorrigeerd worden. Een evidence-based overzicht van alle mogelijke maatregelen, met als besluit een kanttekening over het biologische aspect van nierstenen.
Beste bezoeker, u heeft geen toegang.
Enkel (web)abonnees hebben toegang tot tijdschriftartikelen. Het webabonnement is nog in de maak.
U kunt zich wel alvast (gratis) registreren en tal van andere webartikelen raadplegen!
Auteur
Verschenen in
Referenties
Shoag J, Tasian GE, Goldfarb DS et al. The new epidemiology of nephrolithiasis. Adv Chronic Kidney Dis. 2015 Jul;22(4):273-8
Rendina D, De Filippo G et al. Metabolic syndrome and nephrolithiasis: a systematic review and meta-analysis of the scientific evidence. J Nephrol. 2014 Aug;27(4):371-6
Robertson WG. Dietary recommendations and treatment of patients with recurrent idiopathic calcium stone disease. Urolithiasis. 2016 Feb;44(1):9-26
Prezioso D, Strazzullo P, Lotti T et al. Dietary treatment of urinary risk factors for renal stone formation. A review of CLU Working Group. Arch Ital Urol Androl. 2015 Jul 7;87(2):105-20
Taylor EN, Curhan GC. Determinants of 24-hour urinary oxalate excretion. Clin J Am Soc Nephrol. 2008 Sep;3(5):1453-60
Taylor EN, Curhan GC. Oxalate intake and the risk for nephrolithiasis. J Am Soc Nephrol. 2007 Jul;18(7):2198-204
Traxer O, Huet B, Poindexter J et al. Effect of ascorbic acid consumption on urinary stone risk factors. J Urol. 2003; 170 :397– 401
Taylor EN, Stampfer MJ, Curhan GC. Dietary factors and the risk of incident kidney stones in men: new insights after 14 years of follow-up. J Am Soc Nephrol. 2004; 15 :3225-3232
Ferraro PM, Curhan GC et al. Total, Dietary, and Supplemental Vitamin C Intake and Risk of Incident Kidney Stones. Am J Kidney Dis. 2016 Mar;67(3):400-7
Nguyen QV1, Kälin A, Drouve U et al. Sensitivity to meat protein intake and hyperoxaluria in idiopathic calcium stone formers. Kidney Int. 2001 Jun;59(6):2273-81
Siener R, Bangen U, Sidhu H et al. The role of Oxalobacter formigenes colonization in calcium oxalate stone disease. Kidney Int. 2013 Jun;83(6):1144-9
Mogna L, Pane M, Nicola S et al. Screening of different probiotic strains for their in vitro ability to metabolise oxalates: any prospective use in humans? J Clin Gastroenterol. 2014 Nov-Dec;48 Suppl 1:S91-5
Massey L. Magnesium therapy for nephrolithiasis. Magnes Res. 2005 Jun;18(2):123-6
Phillips R, Hanchanale VS et al. Citrate salts for preventing and treating calcium containing kidney stones in adults. Cochrane Database Syst Rev. 2015 Oct 6;10:CD010057
Eisner BH, Sheth S, Dretler SP et al. High dietary magnesium intake decreases hyperoxaluria in patients with nephrolithiasis. Urology. 2012 Oct;80(4):780-3
Friedlander JI, Antonelli JA, Pearle MS. Diet: from food to stone. World J Urol. 2015 Feb;33(2):179-85
Han H, Segal AM, Seifter JL et al. Nutritional management of kidney stones (nephrolithiasis). Clin Nutr Res. 2015 Jul;4(3):137-52
Nouvenne A, Meschi T, Prati B et al. Effects of a low-salt diet on idiopathic hypercalciuria in calcium-oxalate stone formers: a 3-mo randomized controlled trial. Am J Clin Nutr. 2010 Mar;91(3):565-70
Ticinesi A, Nouvenne A, Maalouf NM et al. Salt and nephrolithiasis. Nephrol Dial Transplant. 2016 Jan;31(1):39-45
Giannini S, Nobile M, Sartori L et al. Acute effects of moderate dietary protein restriction in patients with idiopathic hypercalciuria and calcium nephrolithiasis. Am J Clin Nutr. 1999 Feb;69(2):267-71
Rotily M, Léonetti F, Iovanna C et al. Effects of low animal protein or high-fiber diets on urine composition in calcium nephrolithiasis. Kidney Int. 2000 Mar;57(3):1115-23
Nguyen QV, Kälin A, Drouve U, Casez JP, Jaeger P. Sensitivity to meat protein intake and hyperoxaluria in idiopathic calcium stone formers. Kidney Int. 2001 Jun;59(6):2273-8
Massey LK, Kynast-Gales SA. Diets with either beef or plant proteins reduce risk of calcium oxalate precipitation in patients with a history of calcium kidney stones. J Am Diet Assoc. 2001 Mar;101(3):326-31
Kessler T, Jansen B, Hesse A. Effect of blackcurrant-, cranberry- and plum juice consumption on risk factors associated with kidney stone formation. Eur J Clin Nutr. 2002 Oct;56(10):1020-3
Karagülle O, Smorag U, Candir F et al. Clinical study on the effect of mineral waters containing bicarbonate on the risk of urinary stone formation in patients with multiple episodes of CaOx-urolithiasis. World J Urol. 2007 Jun;25(3):315-23
Pinheiro VB, Baxmann AC, Tiselius HG et al. The effect of sodium bicarbonate upon urinary citrate excretion in calcium stone formers. Urology. 2013 Jul;82(1):33-7
Bruun JM, Maersk M, Belza A et al. Consumption of sucrose-sweetened soft drinks increases plasma levels of uric acid in overweight and obese subjects: a 6-month randomised controlled trial. Eur J Clin Nutr. 2015 Aug;69(8):949-53
Taylor EN, Curhan GC. Fructose consumption and the risk of kidney stones. Kidney Int. 2008 Jan;73(2):207-12
Nguyen NU, Dumoulin G, Henriet MT et al. Increase in urinary calcium and oxalate after fructose infusion. Horm Metab Res. 1995 Mar;27(3):155-8
Nguyen NU, Dumoulin G et al. Urinary calcium and oxalate excretion during oral fructose or glucose load in man. Horm Metab Res. 1989 Feb;21(2):96-9
Ferraro PM, Taylor EN et al. Soda and other beverages and the risk of kidney stones. Clin J Am Soc Nephrol. 2013 Aug;8(8):1389-95
Boonla C, Hunapathed C, Bovornpadungkitti S et al. Messenger RNA expression of monocyte chemoattractant protein-1 and interleukin-6 in stone-containing kidneys. BJU Int. 2008 May;101(9):1170-7
Siener R, Jansen B, Watzer B et al. Effect of n-3 fatty acid supplementation on urinary risk factors for calcium oxalate stone formation. J Urol. 2011 Feb;185(2):719-24
Yasui T, Suzuki S, Itoh Y et al. Eicosapentaenoic acid has a preventive effect on the recurrence of nephrolithiasis. Urol Int. 2008;81(2):135-8
Ortiz-Alvarado O, Miyaoka R, Kriedberg C et al. Omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid in the management of hypercalciuric stone formers. Urology. 2012 Feb;79(2):282-6
Stoller ML, Chi T, Eisner BH et al. Changes in urinary stone risk factors in hypocitraturic calcium oxalate stone formers treated with dietary sodium supplementation. J Urol. 2009 Mar;181(3):1140-4
Domrongkitchaiporn S, Stitchantrakul W, Kochakarn W. Causes of hypocitraturia in recurrent calcium stone formers: focusing on urinary potassium excretion. Am J Kidney Dis. 2006 Oct;48(4):546-54
Kirdpon S, Kirdpon W, Airarat W et al. Effect of aloe (Aloe vera Linn.) on healthy adult volunteers: changes in urinary composition. J Med Assoc Thai. 2006 Aug;89 Suppl 2:S9-14
Brymora A, Flisiński M, Johnson RJ et al. Low-fructose diet lowers blood pressure and inflammation in patients with chronic kidney disease. Nephrol Dial Transplant. 2012 Feb;27(2):608-12
Shi Y, Williamson G. Quercetin lowers plasma uric acid in pre-hyperuricaemic males: a randomised, double-blinded, placebo-controlled, cross-over trial. Br J Nutr. 2016 Mar;115(5):800-6
Manfredini R, De Giorgi A et al. Pears and renal stones: possible weapon for prevention? A comprehensive narrative review. Eur Rev Med Pharmacol Sci. 2016 Feb;20(3):414-25
Naghii MR, Babaei M, Hedayati M. Androgens involvement in the pathogenesis of renal stones formation. PLoS One. 2014 Apr 2;9(4):e93790
Wang H, Man L, Li G et al. Association between serum vitamin D levels and the risk of kidney stone: evidence from a meta-analysis. Nutr J. 2016 Mar 31;15:32
Khan SR. Reactive oxygen species, inflammation and calcium oxalate nephrolithiasis. Transl Androl Urol. 2014 Sep 1;3(3):256-276
Al-Awadi KA, Kehinde EO et al. Treatment of renal calculi by lithotripsy: minimizing short-term shock wave induced renal damage by using antioxidants. Urol Res. 2008 Feb;36(1):51-60
Kehinde EO, Al-Awadi KA, Al-Hunayan A et al. Antioxidant therapy is associated with a reduction in the serum levels of mediators of renal injury following lithotripsy for renal calculi. J Endourol. 2008 Nov;22(11):2537-45
Modi J, Modi P, Pal B et al. Role of Vitamin C and E supplementation in reduction of serum level of renal injury marker following shock wave lithotripsy: Prospective single centre experience. Urol Ann. 2015 Jul-Sep;7(3):350-4
Stern JM, Moazami S, Qiu Y et al. Evidence for a distinct gut microbiome in kidney stone formers compared to non-stone formers. Urolithiasis. 2016 Apr 26. [Epub ahead of print]
Turney BW, Appleby PN, Reynard JM et al. Diet and risk of kidney stones in the Oxford cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC). Eur J Epidemiol. 2014 May;29(5):363-9
Hirayama H, Wang Z, Nishi K et al. Effect of Desmodium styracifolium-triterpenoid on calcium oxalate renal stones. Br J Urol. 1993 Feb;71(2):143-7
Koide T, Yamaguchi S et al. The inhibitory effect of kampou extracts on in vitro calcium oxalate crystallization and in vivo stone formation in an animal model. Int J Urol. 1995 May;2(2):81-6
Lin E, Ho L, Lin MS et al. Wu-Ling-San formula prophylaxis against recurrent calcium oxalate nephrolithiasis - a prospective randomized controlled trial. Afr J Tradit Complement Altern Med. 2013 Aug 12;10(5):199-209
Nishihata M, Kohjimoto Y, Hara I. Effect of Kampo extracts on urinary stone formation: an experimental investigation. Int J Urol. 2013 Oct;20(10):1032-6
Sheng B, He D, Zhao J et al. The protective effects of the traditional Chinese herbs against renal damage induced by extracorporeal shock wave lithotripsy: a clinical study. Urol Res. 2011 Apr;39(2):89-97
Faridi P, Seradj H, Mohammadi-Samani S et al. Randomized and double-blinded clinical trial of the safety and calcium kidney stone dissolving efficacy of Lapis judaicus. J Ethnopharmacol. 2014 Oct 28;156:82-7
Duffin C. Lapis Judaicus or the Jews' stone: The folklore of fossil echinoid spines. Proceedings of the Geologists Association. 2006; 117(3):265-275
Singh RG, Behura SK, Kumar R. Litholytic property of Kulattha (Dolichous biflorus) vs potassium citrate in renal calculus disease: a comparative study. J Assoc Physicians India. 2010 May;58:286-9
Brardi S, Imperiali P, Cevenini G et al. Effects of the association of potassium citrate and agropyrum repens in renal stone treatment: results of a prospective randomized comparison with potassium citrate. Arch Ital Urol Androl. 2012 Jun;84(2):61-7
Boim MA, Heilberg IP, Schor N. Phyllanthus niruri as a promising alternative treatment for nephrolithiasis. Int Braz J Urol. 2010 Nov-Dec;36(6):657-64
Premgamone A, Sriboonlue P et al. A long-term study on the efficacy of a herbal plant, Orthosiphon grandiflorus, and sodium potassium citrate in renal calculi treatment. Southeast Asian J Trop Med Public Health. 2001 Sep;32(3):654-60
Erickson SB, Vrtiska TJ et al. Cystone® for 1 year did not change urine chemistry or decrease stone burden in cystine stone formers. Urol Res. 2011 Jun;39(3):197-203
Erickson SB, Vrtiska TJ, Lieske JC. Effect of Cystone® on urinary composition and stone formation over a one year period. Phytomedicine. 2011 Jul 15;18(10):863-7
Shekar Kumaran MG, Patki PS. Evaluation of an Ayurvedic formulation (Cystone), in urolithiasis: A double blind, placebo-controlled study. Eur J Integr Med. 2011; 3:23-28.
Mohanty NK, Nayak RL, Patki PS. Safety and Efficacy of an Ayurvedic Formulation Cystone in Management of Ureteric Calculi: A Prospective Randomized Placebo Controlled Study. Am J Pharmacol Toxicol. 2010; 5:58-64
Singh RG, Singh TB et al. A comparative pilot study of litholytic properties of Celosia argental (Sitivaraka) versus potassium citrate in renal calculus disease. J Altern Complement Med. 2012 May;18(5):427-8
Patankar S, Dobhada S et al. A prospective, randomized, controlled study to evaluate the efficacy and tolerability of Ayurvedic formulation "varuna and banana stem" in the management of urinary stones. J Altern Complement Med. 2008 Dec;14(10):1287-90
Dinesh V et al. Herbal formulations used in treatment of kidney stone by native folklore of Nizamabad District, Andhra Pradesh, India. Bioscience Discovery. 2013; 4(2):250-253
Chitme HR et al. Herbel treatment for urinary stones. IJPSR. 2010; 1(2):24-31
Nasim MJ, Bin Asad MH, Durr-e-Sabih et al. Gist of medicinal plants of Pakistan having ethnobotanical evidences to crush renal calculi (kidney stones). Acta Pol Pharm. 2014 Jan-Feb;71(1):3-10
Atmani F. Medical management of urolithiasis, what opportunity for phytotherapy? Front Biosci. 2003 May 1;8:s507-14
Grases F, Melero G et al. Urolithiasis and phytotherapy. Int Urol Nephrol. 1994;26(5):507-11