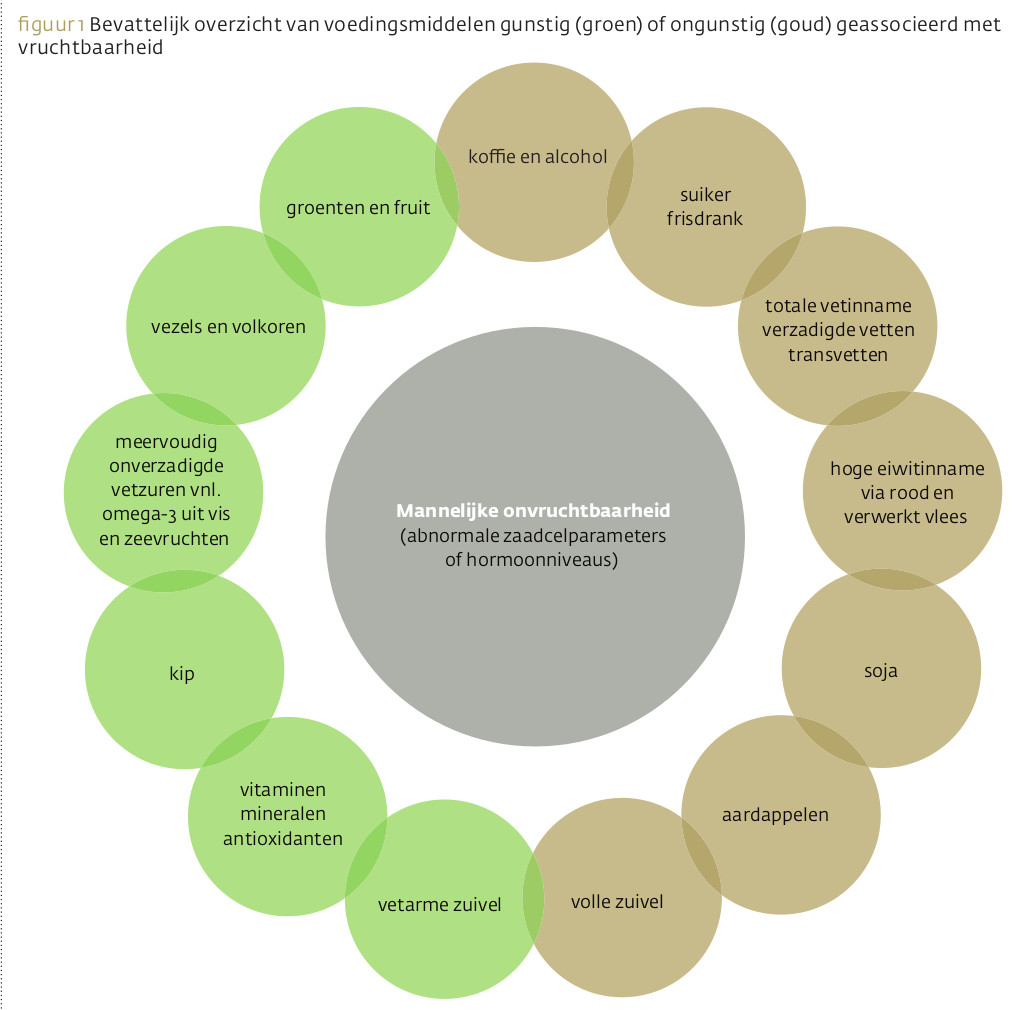
Voeding moeten we beschouwen als een vruchtbaarheidsfactor. Steeds meer evidentie laat zien dat de vruchtbaarheid van de man samenvalt met wat hij eet. Dat laat ook een bespreking van afzonderlijke voedingsstoffen uitschijnen: vele vormen een klein radertje in de complexe ontwikkeling van zaadcellen. De meeste therapieën met voedingssupplementen richten zich op oxidatieve stress en/of bescherming van de celmembranen. Kruiden hebben ook potentieel, zoals blijkt uit een handvol studies.
Beste bezoeker, u heeft geen toegang.
Enkel (web)abonnees hebben toegang tot tijdschriftartikelen. Het webabonnement is nog in de maak.
U kunt zich wel alvast (gratis) registreren en tal van andere webartikelen raadplegen!
Auteur
Verschenen in
Referenties
Salas-Huetos A, Bulló M, Salas-Salvadó J. Dietary patterns, foods and nutrients in male fertility parameters and fecundability: a systematic review of observational studies. Hum Reprod Update. 2017 Jul 1;23(4):371-389
Gaskins AJ, Chavarro JE. Diet and fertility: a review. Am J Obstet Gynecol. 2017 Aug 24. pii: S0002-9378(17)30945-6
Chambers TJ, Richard RA. The impact of obesity on male fertility. Hormones (Athens). 2015 Oct-Dec;14(4):563-8
Yao DF, Mills JN. Male infertility: lifestyle factors and holistic, complementary, and alternative therapies. Asian J Androl. 2016 May-Jun;18(3):410-8
Ricci E, Al-Beitawi S et al. Dietary habits and semen parameters: a systematic narrative review. Andrology. 2018 Jan;6(1):104-116
Cederroth CR, Zimmermann C, Nef S. et al. Soy, phytoestrogens and their impact on reproductive health. Mol Cell Endocrinol. 2012 May 22;355(2):192-200
Ricci E, Viganò P et al. Coffee and caffeine intake and male infertility: a systematic review. Nutr J. 2017 Jun 24;16(1):37
Oostingh EC, Steegers-Theunissen RP et al. Strong adherence to a healthy dietary pattern is associated with better semen quality, especially in men with poor semen quality. Fertil Steril. 2017 Apr;107(4):916-923.e2
Afeiche MC, Williams PL et al. Meat intake and reproductive parameters among young men. Epidemiology. 2014 May;25(3):323-30
Mínguez-Alarcón L, Afeiche MC et al. Hair mercury (Hg) levels, fish consumption and semen parameters among men attending a fertility center. Int J Hyg Environ Health. 2017 Oct 28. pii: S1438-4639(17)30315-2
Showell MG, Mackenzie-Proctor R et al. Antioxidants for male subfertility. Cochrane Database Syst Rev. 2014;(12):CD007411
Wright C, Milne S, Leeson H. Sperm DNA damage caused by oxidative stress: modifiable clinical, lifestyle and nutritional factors in male infertility. Reprod Biomed Online. 2014 Jun;28(6):684-703
Fraga CG, Motchnik PA et al. Ascorbic acid protects against endogenous oxidative DNA damage in human sperm. Proc Natl Acad Sci U S A. 1991 Dec 15;88(24):11003-6
Greco E, Iacobelli M et al. Reduction of the incidence of sperm DNA fragmentation by oral antioxidant treatment. J Androl. 2005 May-Jun;26(3):349-53
Akmal M, Qadri JQ et al. Improvement in human semen quality after oral supplementation of vitamin C. J Med Food. 2006 Fall;9(3):440-2
Rolf C, Cooper TG et al. Antioxidant treatment of patients with asthenozoospermia or moderate oligoasthenozoospermia with high-dose vitamin C and vitamin E: a randomized, placebo-controlled, double-blind study. Hum Reprod. 1999 Apr;14(4):1028-33.
Rafiee B, Morowvat MH, Rahimi-Ghalati N.Comparing the effectiveness of dietary vitamin c and exercise interventions on fertility parameters in normal obese men. Urol J. 2016 Apr 16;13(2):2635-9
Greco E, Romano S et al. ICSI in cases of sperm DNA damage: beneficial effect of oral antioxidant treatment. Hum Reprod. 2005 Sep;20(9):2590-4
Alshahrani S. Nutritional Supplementation for the Treatment of Male Infertility. (2015) In book: Nutrition, Fertility, and Human Reproductive Function, Publisher: TheTaylor & Francis Group
Safarinejad MR, Safarinejad S. Efficacy of selenium and/or N-acetyl-cysteine for improving semen parameters in infertile men: a double-blind, placebo controlled, randomized study. J Urol. 2009 Feb;181(2):741-51. doi: 10.1016/j.juro.2008.10.015. Epub 2008 Dec 16.
Scott R, MacPherson A et al. The effect of oral selenium supplementation on human sperm motility. Br J Urol. 1998 Jul;82(1):76-80.
Omu AE, Al-Azemi MK et al. Indications of the mechanisms involved in improved sperm parameters by zinc therapy. Med Princ Pract. 2008;17(2):108-16.
Hadwan MH, Almashhedy LA, Alsalman AR. Study of the effects of oral zinc supplementation on peroxynitrite levels, arginase activity and NO synthase activity in seminal plasma of Iraqi asthenospermic patients. Reprod Biol Endocrinol. 2014 Jan 3;12:1
Raigani M, Yaghmaei B et al. The micronutrient supplements, zinc sulphate and folic acid, did not ameliorate sperm functional parameters in oligoasthenoteratozoospermic men. Andrologia. 2014;46(9):956-62
Ahmed SD, Karira KA et al. Role of L-carnitine in male infertility. J Pak Med Assoc. 2011 Aug;61(8):732-6
Sofimajidpour H, Ghaderi E, Ganji O. Comparison of the effects of varicocelectomy and oral L-carnitine on sperm parameters in infertile men with varicocele. J Clin Diagn Res. 2016 Apr;10(4):PC07-10
Moslemi Mehni N, Ketabchi AA, Hosseini E. Combination effect of Pentoxifylline and L-carnitine on idiopathic oligoasthenoteratozoospermia. Iran J Reprod Med. 2014 Dec;12(12):817-24.
Sigman M, Glass S et al. Carnitine for the treatment of idiopathic asthenospermia: a randomized, double-blind, placebo-controlled trial. Fertil Steril. 2006 May;85(5):1409-14
Lafuente R, González-Comadrán M et al. Coenzyme Q10 and male infertility: a meta-analysis. J Assist Reprod Genet. 2013 Sep;30(9):1147-56
Kobori Y, Ota S et al. Antioxidant cosupplementation therapy with vitamin C, vitamin E, and coenzyme Q10 in patients with oligoasthenozoospermia. Arch Ital Urol Androl. 2014 Mar 28;86(1):1-4
Nadjarzadeh A, Shidfar F et al. Effect of Coenzyme Q10 supplementation on antioxidant enzymes activity and oxidative stress of seminal plasma: a double-blind randomised clinical trial. Andrologia. 2014 Mar;46(2):177-83
Haghighian HK, Haidari F et al. Randomized, triple-blind, placebo-controlled clinical trial examining the effects of alpha-lipoic acid supplement on the spermatogram and seminal oxidative stress in infertile men. Fertil Steril. 2015 Aug;104(2):318-24.
Ghyasvand T, Goodarzi MT et al. Serum levels of lycopene, beta-carotene, and retinol and their correlation with sperm DNA damage in normospermic and infertile men. Int J Reprod Biomed (Yazd). 2015 Dec;13(12):787-92.
Durairajanayagam D, Agarwal A et al. Lycopene and male infertility. Asian J Androl. 2014 May-Jun;16(3):420-5
Gupta NP, Kumar R. Lycopene therapy in idiopathic male infertility--a preliminary report. Int Urol Nephrol. 2002;34:369–72
Mohanty N, Kumar S, Jha A, Arora R. Management of idiopathic oligoasthenospermia with lycopene. Indian J Urol. 2001;18:57–61.
Yamamoto Y, Aizawa K et al. The effects of tomato juice on male infertility. Asia Pac J Clin Nutr. 2017 Jan;26(1):65-71
Comhaire FH, El Garem Y et al. Combined conventional/antioxidant "Astaxanthin" treatment for male infertility: a double blind, randomized trial. Asian J Androl. 2005 Sep;7(3):257-62.
Safarinejad MR, Shafiei N, Safarinejad S. A prospective double-blind randomized placebo-controlled study of the effect of saffron (Crocus sativus Linn.) on semen parameters and seminal plasma antioxidant capacity in infertile men with idiopathic oligoasthenoteratozoospermia. Phytother Res. 2011 Apr;25(4):508-16
Esmaeili V, Shahverdi AH et al. Dietary fatty acids affect semen quality: a review. Andrology. 2015 May;3(3):450-61
Martínez-Soto JC, Landeras J, Gadea J. Spermatozoa and seminal plasma fatty acids as predictors of cryopreservation success. Andrology. 2013 May;1(3):365-75
Safarinejad MR. Effect of omega-3 polyunsaturated fatty acid supplementation on semen profile and enzymatic anti-oxidant capacity of seminal plasma in infertile men with idiopathic oligoasthenoteratospermia: a double-blind, placebo-controlled, randomised study. Andrologia. 2011 Feb;43(1):38-47
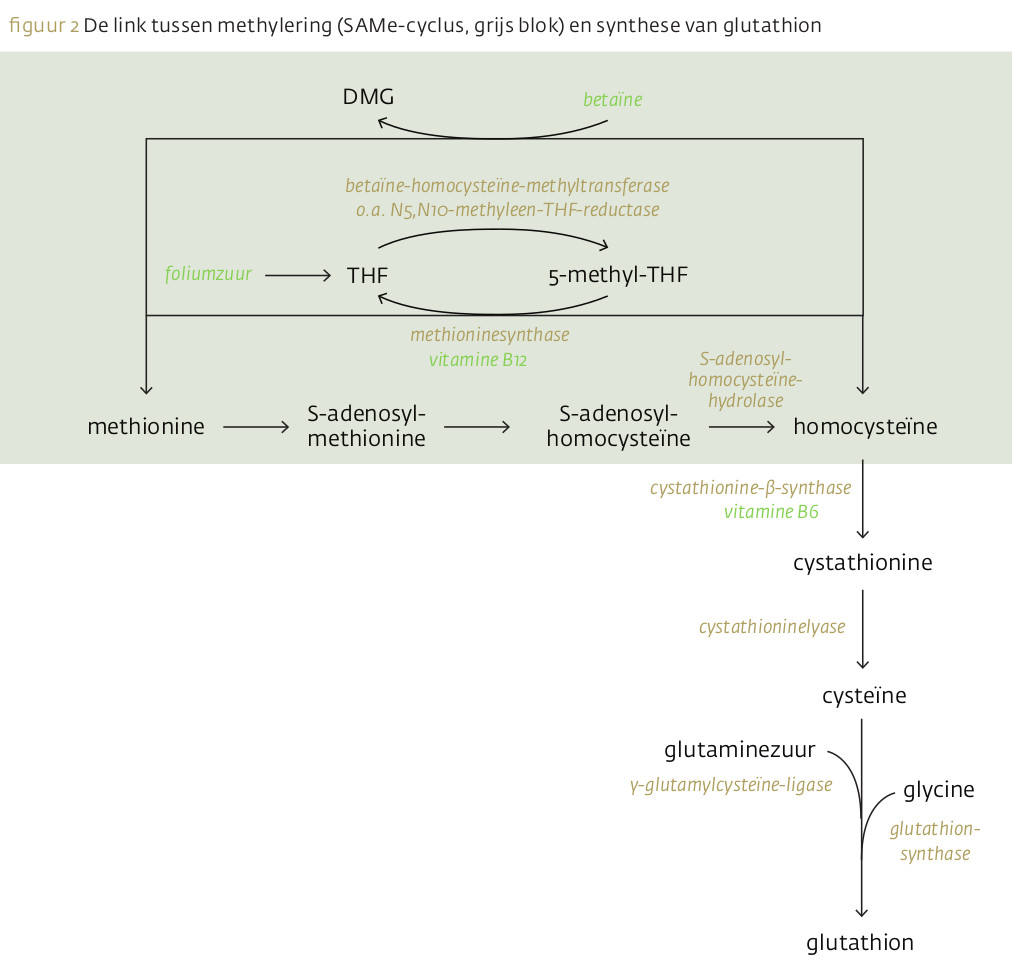
Dattilo M, Cornet D et al. The importance of the one carbon cycle nutritional support in human male fertility: a preliminary clinical report. Reprod Biol Endocrinol. 2014 Jul 29;12:71
Najafipour R, Moghbelinejad S et al. Effect of B9 and B12 vitamin intake on semen parameters and fertility of men with MTHFR polymorphisms. Andrology. 2017 Jul;5(4):704-710
Condorelli RA, La Vignera S et al. Myo-inositol as a male fertility molecule: speed them up! Eur Rev Med Pharmacol Sci. 2017 Jun;21(2 Suppl):30-35
Gulino FA, Leonardi E et al. Effect of treatment with myo-inositol on semen parameters of patients undergoing an IVF cycle: in vivo study. Gynecol Endocrinol. 2016;32(1):65-8
Calogero AE, Gullo G et al. Myoinositol improves sperm parameters and serum reproductive hormones in patients with idiopathic infertility: a prospective double-blind randomized placebo-controlled study. Andrology. 2015 May;3(3):491-5
Shannon J, El Saigh I et al. Usage of herbal medications in patients undergoing IVF treatment in an Irish infertility treatment unit. Ir J Med Sci. 2010 Mar;179(1):63-5
Salvati G, Genovesi G et al. Effects of Panax Ginseng C.A. Meyer saponins on male fertility. Panminerva Med. 1996 Dec;38(4):249-54.
Park HJ, Choe S, Park NC. Effects of Korean red ginseng on semen parameters in male infertility patients: A randomized, placebo-controlled, double-blind clinical study. Chin J Integr Med. 2016 Jul;22(7):490-5
Lee MS, Lee HW et al. The use of maca (Lepidium meyenii) to improve semen quality: A systematic review. Maturitas. 2016 Oct;92:64-69
Hosseini J, Mardi Mamaghani A et al. The influence of ginger (Zingiber officinale) on human sperm quality and DNA fragmentation: A double-blind randomized clinical trial. Int J Reprod Biomed (Yazd). 2016 Aug;14(8):533-40.
Khani B, Bidgoli SR et al. Effect of sesame on sperm quality of infertile men. J Res Med Sci. 2013 Mar;18(3):184-7.
Kolahdooz M, Nasri S et al. Effects of Nigella sativa L. seed oil on abnormal semen quality in infertile men: a randomized, double-blind, placebo-controlled clinical trial. Phytomedicine. 2014 May 15;21(6):901-5
Tahvilzadeh M, Hajimahmoodi M et al. An evidence-based approach to medicinal plants for the treatment of sperm abnormalities in traditional Persian medicine. Andrologia. 2016 Oct;48(8):860-79
Alizadeh F, Javadi M et al. Curcumin nanomicelle improves semen parameters, oxidative stress, inflammatory biomarkers, and reproductive hormones in infertile men: A randomized clinical trial. Phytother Res. 2017 Nov 28. doi: 10.1002/ptr.5998
Gao D, Cui Y et al. Effect of traditional Chinese medicine on oligoasthenospermatism: a narrative review. J Tradit Chin Med. 2014 Oct;34(5):616-20.
Hajizadeh Maleki B, Tartibian B. Moderate aerobic exercise training for improving reproductive function in infertile patients: A randomized controlled trial. Cytokine. 2017 Apr;92:55-67
Hajizadeh Maleki B, Tartibian B. Combined aerobic and resistance exercise training for improving reproductive function in infertile men: a randomized controlled trial. Appl Physiol Nutr Metab. 2017 Dec;42(12):1293-1306
Abad C, Amengual M et al. Effects of oral antioxidant treatment upon the dynamics of human sperm DNA fragmentation and subpopulations of sperm with highly degraded DNA. Andrologia. 2013 Jun;45(3):211-6