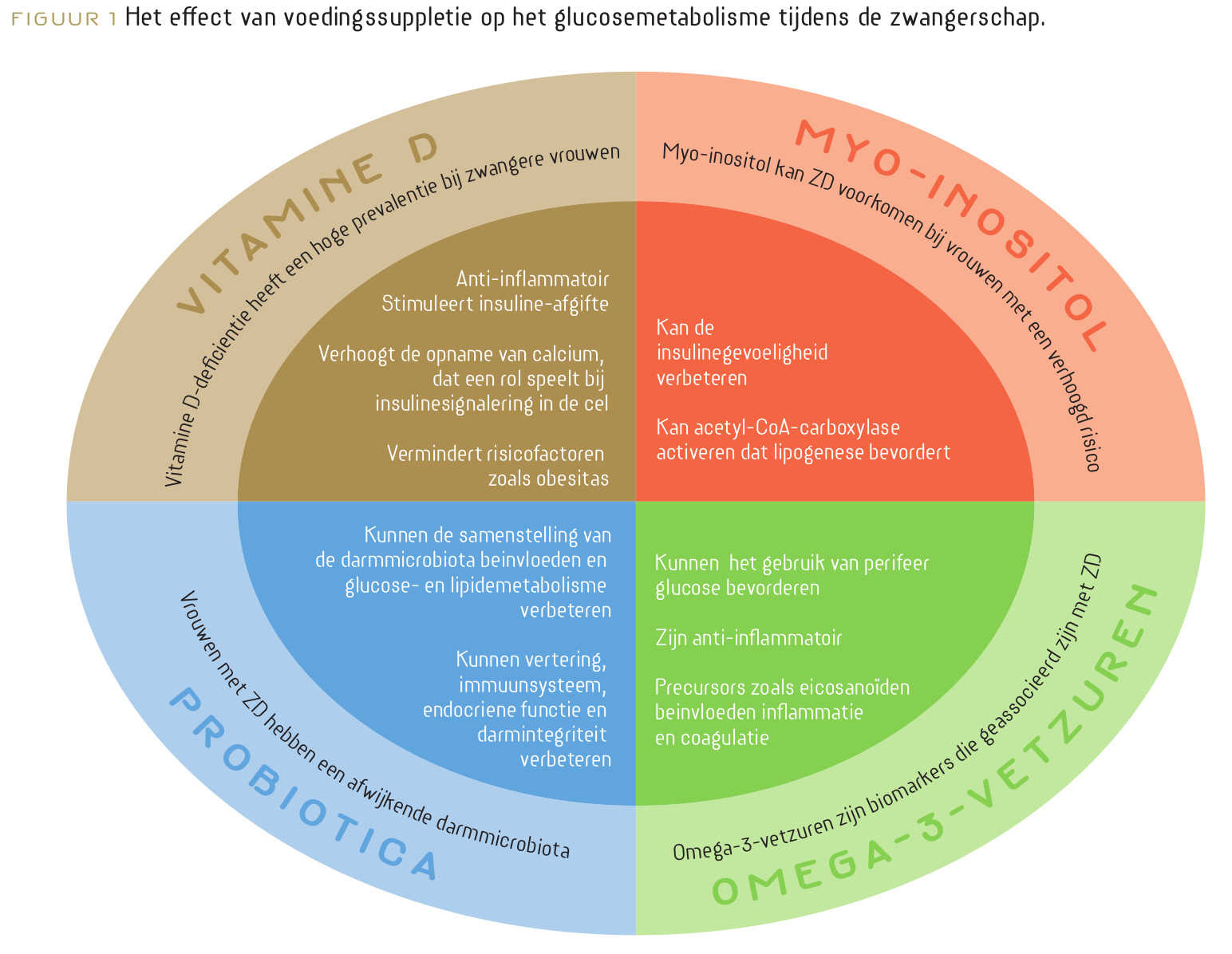
Zwangerschapsdiabetes (ZD) is de meest voorkomende complicatie tijdens de zwangerschap en is geassocieerd met een aanzienlijke morbiditeit bij moeder en foetus. De voedingsstatus van de vrouw voor en tijdens de zwangerschap heeft een cruciale invloed op de gezondheid van de vrouw en op de ontwikkeling en groei van de baby.
Beste bezoeker, u heeft geen toegang.
Enkel (web)abonnees hebben toegang tot tijdschriftartikelen. Het webabonnement is nog in de maak.
U kunt zich wel alvast (gratis) registreren en tal van andere webartikelen raadplegen!
Auteur
Verschenen in
Referenties
Damm P, Houshmand-Oeregaard A, Kelstrup L, et al. Gestational diabetes mellitus and long-term consequences for mother and offspring: a view from Denmark. Diabetologia. 2016;59(7):1396-1399.
Raghavan R, Dreibelbis C, Kingshipp BL, et al. Dietary patterns before and during pregnancy and maternal outcomes: a systematic review. Am J Clin Nutr. 2019;109(Supplement_1):705S-728S.
Asadi M, Shahzeidi M, Nadjarzadeh A, et al. The relationship between pre‐pregnancy dietary patterns adherence and risk of gestational diabetes mellitus in Iran: A case–control study. Nutr Diet. 2019;76(5):597-603.
Kimmons JE, Blanck HM, Tohill BC, et al. Associations between body mass index and the prevalence of low micronutrient levels among US adults. Medscape Gen Med. 2006;8(4):59.
Person OK, Person B, Szomstein S, et al. Nutritional Deficiency in Morbidity Obese patients: A new form of malnutrition. Obese Surg. 2008;18:1028-1034.
Dualib PM, Ogassavara J, Mattar R, et al. Gut microbiota and gestational Diabetes Mellitus: A systematic review. Diabetes Res Clin Pract. 2021;180:109078.
Seth A, Yan F, Polk DB, et al. Probiotics ameliorate the hydrogen peroxide-induced epithelial barrier disruption by a PKC-and MAP kinase-dependent mechanism. Am J Physiol Liver Physiol. 2008;294(4):G1060-G1069.
Jones SE, Versalovic J. Probiotic Lactobacillus reuteribiofilms produce antimicrobial and anti-inflammatory factors. BMC Microbiol. 2009;9(1):1-9.
Amabebe E, Anumba DOC. Female gut and genital tract microbiota-induced crosstalk and differential effects of short-chain fatty acids on immune sequelae. Front Immunol. Published online 2020:2184.
Amabebe E, Robert FO, Agbalalah T, et al. Microbial dysbiosis-induced obesity: role of gut microbiota in homoeostasis of energy metabolism. Br J Nutr. 2020;123(10):1127-1137.
Chen Y, Yue R, Zhang B, et al. Effects of probiotics on blood glucose, biomarkers of inflammation and oxidative stress in pregnant women with gestational diabetes mellitus: A meta-analysis of randomized controlled trials. Med Clínica (English Ed. 2020;154(6):199-206.
Zhang J, Ma S, Wu S, et al. Effects of probiotic supplement in pregnant women with gestational diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. J Diabetes Res. 2019;2019.
Homayouni A, Bagheri N, Mohammad-Alizadeh-Charandabi S, et al. Prevention of gestational diabetes mellitus (GDM) and probiotics: mechanism of action: a review. Curr Diabetes Rev. 2020;16(6):538-545.
VandeVusse L, Hanson L, Safdar N. Perinatal outcomes of prenatal probiotic and prebiotic administration: an integrative review. J Perinat Neonatal Nurs. 2013;27(4):288-301.
Dallanora S, Medeiros de Souza Y, Deon RG, et al. Do probiotics effectively ameliorate glycemic control during gestational diabetes? A systematic review. Arch Gynecol Obstet. 2018;298(3):477-485.
Callaway LK, McIntyre HD, Barrett HL, et al. Probiotics for the prevention of gestational diabetes mellitus in overweight and obese women: findings from the SPRING double-blind randomized controlled trial. Diabetes Care. 2019;42(3):364-371.
Pellonperä O, Mokkala K, Houttu N, et al. Efficacy of fish oil and/or probiotic intervention on the incidence of gestational diabetes mellitus in an at-risk group of overweight and obese women: a randomized, placebo-controlled, double-blind clinical trial. Diabetes Care. 2019;42(6):1009-1017.
Yanai H, Hamasaki H, Katsuyama H, et al. Effects of intake of fish or fish oils on the development of diabetes. J Clin Med Res. 2015;7(1):8.
Patel PS, Sharp SJ, Luben RN, et al. Association between type of dietary fish and seafood intake and the risk of incident type 2 diabetes: the European prospective investigation of cancer (EPIC)-Norfolk cohort study. Diabetes Care. 2009;32(10):1857-1863.
Itsiopoulos C, Marx W, Mayr HL, et al. The role of omega-3 polyunsaturated fatty acid supplementation in the management of type 2 diabetes mellitus: A narrative review. J Nutr Intermed Metab. 2018;14:42-51.
Fedor D, Kelley DS. Prevention of insulin resistance by n-3 polyunsaturated fatty acids. Curr Opin Clin Nutr Metab Care. 2009;12(2):138-146.
Cooper JA, Stevenson JL, Paton CM. Hunger and satiety responses to saturated fat‐rich meals before and after a high PUFA diet. FASEB J. 2016;30:405-407.
Herrera E, Ortega-Senovilla H. Implications of lipids in neonatal body weight and fat mass in gestational diabetic mothers and non-diabetic controls. Curr Diab Rep. 2018;18(2):1-13.
Toescu V, Nuttall SL, Martin U, et al. Changes in plasma lipids and markers of oxidative stress in normal pregnancy and pregnancies complicated by diabetes. Clin Sci. 2004;106(1):93-98.
Schaefer-Graf UM, Graf K, Kulbacka I, et al. Maternal lipids as strong determinants of fetal environment and growth in pregnancies with gestational diabetes mellitus. Diabetes Care. 2008;31(9):1858-1863.
De‐Regil LM, Peña‐Rosas JP, Fernández‐Gaxiola AC, et al. Effects and safety of periconceptional oral folate supplementation for preventing birth defects. Cochrane database Syst Rev. 2015;(12).
Son GH, Kwon JY, Kim YH, et al. Maternal serum triglycerides as predictive factors for large-for-gestational age newborns in women with gestational diabetes mellitus. Acta Obstet Gynecol Scand. 2010;89(5):700-704.
Simeonova-Krstevska S, Velkoska-Nakova M, Lega MH, et al. Effect of lipid parameters on foetal growth in gestational diabetes mellitus pregnancies. Pril (Makedonska Akad na Nauk i Umet Oddelenie za Med Nauki). 2014;35(2):131-6.
Jamilian M, Samimi M, Ebrahimi FA, et al. The effects of vitamin D and omega-3 fatty acid co-supplementation on glycemic control and lipid concentrations in patients with gestational diabetes. J Clin Lipidol. 2017;11(2):459-468.
Bhatt DL, Steg PG, Miller M, et al. Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med. 2019;380(1):11-22.
Contreras-Duarte S, Carvajal L, Garchitorena MJ, et al. Gestational diabetes mellitus treatment schemes modify maternal plasma cholesterol levels dependent to women s weight: Possible impact on feto-placental vascular function. Nutrients. 2020;12(2):506.
Middleton P, Gomersall JC, Gould JF, et al. Omega‐3 fatty acid addition during pregnancy. Cochrane Database Syst Rev. 2018;(11).
Ji X, Grandner MA, Liu J. The relationship between micronutrient status and sleep patterns: a systematic review. Public Health Nutr. 2016;20(4):687-701.
Wei S-Q, Qi H-P, Luo Z-C, et al. Maternal vitamin D status and adverse pregnancy outcomes: a systematic review and meta-analysis. J Matern Neonatal Med. 2013;26(9):889-899.
Wilson RL, Leviton AJ, Leemaqz SY, et al. Vitamin D levels in an Australian and New Zealand cohort and the association with pregnancy outcome. BMC Pregnancy Childbirth. 2018;18(1):1-10.
Ojo O, Weldon SM, Thompson T, et al. The effect of vitamin D supplementation on glycaemic control in women with gestational diabetes mellitus: a systematic review and meta-analysis of randomised controlled trials. Int J Environ Res Public Health. 2019;16(10):1716.
Yin W, Jin D, Yao M, et al. Effect of vitamin D supplementation on gestational diabetes mellitus: a Meta-analysis. Wei Sheng Yan Jiu. 2019;48(5):811-821.
Corcoy R, Mendoza LC, Simmons D, et al. The DALI vitamin D randomized controlled trial for gestational diabetes mellitus prevention: No major benefit shown besides vitamin D sufficiency. Clin Nutr. 2020;39(3):976-984.
Jamilian M, Mirhosseini N, Eslahi M, et al. The effects of magnesium-zinc-calcium-vitamin D co-supplementation on biomarkers of inflammation, oxidative stress and pregnancy outcomes in gestational diabetes. BMC Pregnancy Childbirth. 2019;19(1):1-8.
Jin S, Sha L, Dong J, et al. Effects of nutritional strategies on glucose homeostasis in gestational diabetes mellitus: a systematic review and network meta-analysis. J Diabetes Res. 2020;2020.
Caputo M, Bona E, Leone I, et al. Inositols and metabolic disorders: From farm to bedside. J Tradit Complement Med. 2020;10(3):252-259.
Larner J, Brautigan DL, Thorner MO. D-chiro-inositol glycans in insulin signaling and insulin resistance. Mol Med. 2010;16(11):543-552.
Bizzarri M, Carlomagno G. Inositol: history of an effective therapy for polycystic ovary syndrome. Eur Rev Med Pharmacol Sci. 2014;18(13):1896-1903.
D’Anna R, Scilipoti A, Giordano D, et al. Myo-inositol supplementation and onset of gestational diabetes mellitus in pregnant women with a family history of type 2 diabetes: a prospective, randomized, placebo-controlled study. Diabetes Care. 2013;36(4):854-857.
D’Anna R, Di Benedetto A, Scilipoti A, et al. Myo-inositol supplementation for prevention of gestational diabetes in obese pregnant women: a randomized controlled trial. Obstet Gynecol. 2015;126(2):310-315.
Zhang H, Lv Y, Li Z, et al. The efficacy of myo-inositol supplementation to prevent gestational diabetes onset: a meta-analysis of randomized controlled trials. J Matern Neonatal Med. 2019;32(13):2249-2255.
Crawford TJ, Crowther CA, Alsweiler J, et al. Antenatal dietary supplementation with myo‐inositol in women during pregnancy for preventing gestational diabetes. Cochrane Database Syst Rev. 2015;(12).
Veronese N, Watutantrige-Fernando S, Luchini C, et al. Effect of magnesium supplementation on glucose metabolism in people with or at risk of diabetes: a systematic review and meta-analysis of double-blind randomized controlled trials. Eur J Clin Nutr. 2016;70(12):1354-1359.
Jamilian M, Samimi M, Faraneh AE, et al. Magnesium supplementation affects gene expression related to insulin and lipid in patients with gestational diabetes. Magnes Res. 2017;30(3):71-79.
Ahmadi S, Naderifar M, Samimi M, et al. The effects of magnesium supplementation on gene expression related to inflammatory markers, vascular endothelial growth factor, and pregnancy outcomes in patients with gestational diabetes. Magnes Res. 2018;31(4):131-142.
Bo S, Lezo A, Menato G, et al. Gestational hyperglycemia, zinc, selenium, and antioxidant vitamins. Nutrition. 2005;21(2):186-191.
Iqbal S, Ali I, Rust P, et al. Selenium, zinc, and manganese status in pregnant women and its relation to maternal and child complications. Nutrients. 2020;12(3):725.
Askari G, Iraj B, Salehi-Abargouei A, et al. The association between serum selenium and gestational diabetes mellitus: a systematic review and meta-analysis. J trace Elem Med Biol. 2015;29:195-201.
Wilson RL, Grieger JA, Bianco-Miotto T, et al. Association between maternal zinc status, dietary zinc intake and pregnancy complications: a systematic review. Nutrients. 2016;8(10):641.
Carducci B, Keats EC, Bhutta ZA. Zinc supplementation for improving pregnancy and infant outcome. Cochrane Database Syst Rev. 2021;(3).
Tiongco RE, Arceo E, Clemente B, et al. Association of maternal iron deficiency anemia with the risk of gestational diabetes mellitus: a meta-analysis. Arch Gynecol Obstet. 2019;299(1):89-95.