Eind 2019 maakte de wereld kennis met een nieuw type coronavirus – COVID-19 – dat het acute respiratory distress syndrome of multi-orgaanfalen veroorzaakt, vooral bij kwetsbare individuen zoals immuunverzwakte patiënten, diabetici, ouderen en obese personen. Voorlopige gegevens geven aan dat personen met obesitas een verhoogd risico lopen om ernstige ziektesymptomen van COVID-19 te ontwikkelen, met tot gevolg intensive care en overlijden.1 Leptine, afgegeven door vetweefsel, is bij mensen met overgewicht in grote hoeveelheid aanwezig en verhoogt het ontstekingsmilieu met een ontregeling van de immuunrespons.2 Resveratrol heeft een belangrijk therapeutisch potentieel vanwege zijn ontstekingsremmende en antivirale werkingsmechanismen.48,56,62,63,65,69
Beste bezoeker, u heeft geen toegang.
Enkel (web)abonnees hebben toegang tot tijdschriftartikelen. Het webabonnement is nog in de maak.
U kunt zich wel alvast (gratis) registreren en tal van andere webartikelen raadplegen!
Auteur
Trefwoorden:
Verschenen in
Referenties
1. Albashir A A D. The potential impacts of obesity on COVID-19. Clin Med (Lond). 2020 Jul;20(4):e109-e113.
2. Di Renzo L et al. COVID-19: Is there a role for immunonutrition in obese patient? J Transl Med. 2020 Nov 7;18(1):415.
3. Friedman J M et al. Leptin and the regulation of body weight in mammals. Nature.1998, 395, 763-70.
4. Flament-Durand. The hypothalamus: anatomy and functions. Acta Psychiatr Belg. Jul-Aug 1980;80(4):364-75.
5. Neira Sáinz et al. Leptin resistance and diet-induced obesity: central and peripheral actions of leptin. 2015 Jan;64(1):35-46.
6. Pasarica et al. Reduced adipose tissue oxygenation in human obesity: evidence for rarefaction, macrophage chemotaxis, and inflammation without an angiogenic response. Diabetes. 2009 Mar;58(3):718-25. doi: 10.2337/db08-1098. Epub 2008 Dec 15.
7. Ye J et al. Hypoxia is a potential risk factor for chronic inflammation and adiponectin reduction in adipose tissue of ob/ob and dietary obese mice. Am J Physiol. 2007 Oct;293(4):E1118-28.
8. Andersen C J et al. Impact of Obesity and Metabolic Syndrome on Immunity. Adv Nutr. 2016 Jan 15;7(1):66-75.
9. Martin S S et al. Leptin Resistance: A Possible Interface of Inflammation and Metabolism in Obesity-Related Cardiovascular Disease. J Am Coll Cardiol. 2008 Oct 7; 52(15): 1201–1210.
10. La Cava A et al. The weight of leptin in immunity. Rev Immunol. 2004 May;4(5):371-9.
11. Luzi L et al. Influenza and obesity: its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol. 2020.
12. Honce R et al. Impact of obesity on influenza A virus pathogenesis, immune response, and evolution. Front Immunol. 2019;10(May):1-15.
13. Fu S et al. Leptin Promotes IL-18 Secretion by Activating the NLRP3 Inflammasome in RAW 264.7 Cells. Molecular Medicine Reports 16, nr. 6 (December 2017): 9770–76.
14. Broz P et al. Inflammasomes: mechanism of assembly, regulation and signaling. Nat Rev Immunol. 2016 Jul;16(7):407-20.
15. Liu J et al. The Leptin Resistance. Adv Exp Med Biol. 2018;1090:145-163.
16. Janeway C A et al. Immunobiology: the immune system in health and disease, 6thedition. Churchill Livingstone, 2005.
17. Matarese G et al. Leptin in autoimmunity: many questions, some answers. Tissue Antigens.,2007, 70, 87-95
18. Leem J et al. Interaction between mitochondria and the endoplasmic reticulum: implications for the pathogenesis of type 2-diabetes mellitus. Experimental Diabetes Research 2012; 1-8.
19. Lafontan M. et al. Impact of visceral adipose tissue on liver metabolism part 1: heterogenety of adipose tissue and functional properties of visceral adipose tissue. Diabetes & Metabolism; 2008; 34,317–327.
20. The University of North Carolina at Chapel Hill. Obesity linked with higher risk for COVID-19 complications. University Communications, Wednesday, August 26th, 2020
21. Holick M F. The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention. Rev Endocr Metab Disord. 2017 Jun;18(2):153-165.
22. Ali N. Role of vitamin D in preventing of COVID-19 infection, progression and severity. J Infect Public Health. 2020 Oct;13(10):1373-1380.
23. Yanai H et al. Beneficial Effects of Adiponectin on Glucose and Lipid Metabolism and Atherosclerotic Progression: Mechanisms and Perspectives. 2019 Mar 8;20(5):1190.
24. Soo Lim et al. Insulin-sensitizing effects of exercise on adiponectin and retinol-binding protein-4 concentrations in young and middle-aged women. J Clin Endocrinol Metab. 2008 Jun;93(6):2263-8.
25. Takahashi H et al. TGF-β2 is an exercise-induced adipokine that regulates glucose and fatty acid metabolism. Nature Metabolism volume 1; 2019: 291–303.
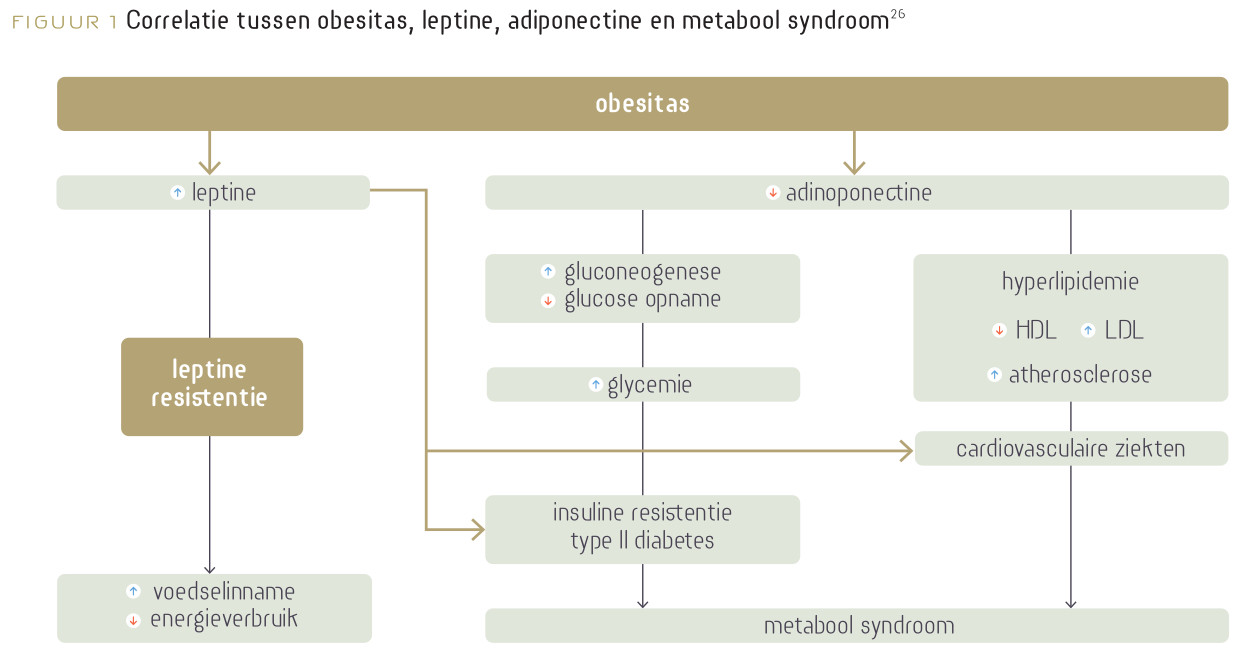
26. Ricci R, Bevilacqua F. The potential role of leptin and adiponectin in obesity: a comparative review. Vet J . 2012 Mar;191(3):292-8.
27. Ackermann M et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in COVID-19. N Engl J Med 2020; 383:120-128.
28. Li W. et al. Angiotensin- converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003; 426 (6965): 450-454.
29. Varga et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020; 395:1417-1418.
30. Jacobs M et al. Increased expression of ACE2,the SARS-CoV-2 entry receptor, in alveolar and bronchial epithelium of smokers and COPD subjects. Eur Respir J 2020; 56: 2002378.
31. Kuba K et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS Coronavirus-induced lung injury. Nature Medicine 2005; 11 (8): 875–9.
32. Bornstein S R et al. Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol. 2020 Jun; 8(6): 546–550.
33. Srivastava P et al. Imbalance between Angiotensin II – Angiotensin (1–7) system is associated with vascular endothelial dysfunction and inflammation in type 2 diabetes with newly diagnosed hypertension. Diabetes Metab Syndr 2019; 13 (3): 2061–8.
34. de Man F S et al. Dysregulated Renin–Angiotensin–Aldosterone System Contributes to Pulmonary Arterial Hypertension. American Journal of Respiratory and Critical Care Medicine 2012; List of Issues; Volume 186, Issue 8.
35. Ingelfinger J R et al. ACE2: A New Target for Prevention of Diabetic Nephropathy? JASN November 2006; 17(11): 2957-2959.
36. Palau V et al. ADAM17 inhibition may exert a protective effect on COVID-19. Nephrology Dialysis Transplantation. Volume 35; Issue 6; June 2020; 1071–1072.
37. Stiefelhagen. Je höher der Blutzucker, desto gefährlicher die SARS-CoV-2-Infektion COVID-19 bei Diabetikern. MMW Fortschr Med. 2020; 162(20): 15–17.
38. Franco J G et al. Resveratrol prevents hyperleptinemia and central leptin resistance in adult rats programmed by early weaning. Horm Metab Res. 2014 Sep;46(10): 728-35.
39. Ardid-Ruiz A et al. Resveratrol Treatment Enhances the Cellular Response to Leptin by Increasing OBRb Content in Palmitate-Induced Steatotic HepG2 Cells. Int J Mol Sci. 2019 Dec; 20(24): 6282.
40. Eseberri et al. Resveratrol Metabolites Modify Adipokine Expression and Secretion in 3T3-L1 Pre-Adipocytes and Mature Adipocytes. PloS One 8; nr. 5 (2013): e63918.
41. Evans H M et al. Effects of resveratrol on cognitive performance, mood and cerebrovascular function in post-menopausal women; a 14-week randomised placebo-controlled intervention trial. Nutrients. 2017; 9(1), 27.
42. Timmers S. et al. Calorie restriction-like effects of 30 days of resveratrol supplementation on energy metabolism and metabolic profile in obese humans. Cell metabolism. 2011, 14(5), 612-622.
43. Ingram D et al. Calorie restriction mimetics: an emerging research field. Aging Cell. 2006 Apr;5(2):97-108.
44. de Ligt M et al. Resveratrol and obesity: Can resveratrol relieve metabolic disturbances? Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease. Nov. 2014,1852(6)
45. Eun Nim Kim et al. The protective effect of resveratrol on vascular aging by modulation of the renin-angiotensin system. Atherosclerosis. 2018 Mar;270:123-131.
46. Horne JR, Vohl MC. Biological plausibility for interactions between dietary fat, resveratrol, ACE2, and SARS-CoV illness severit. Am J Physiol Endocrinol Metab. 2020 May 1;318(5):E830-E833.
47. McLachlan CS. The angiotensin-converting enzyme 2 (ACE2) receptor in the prevention and treatment of COVID-19 are distinctly different paradigms. Clin Hypertens. 2020 Jul 15;26:14.
48. Ramdani LH, Bachari K. Potential therapeutic effects of Resveratrol against SARS-CoV-2, Acta Virol, 2020;64(3):276-280.
49. Szewczuk et al. Resveratrol is a peroxidase-mediated inactivator of COX-1 but not COX-2: a mechanistic approach to the design of COX-1 selective agents. J Biol Chem. 2004 May 21;279 (21): 2727-37.
50. Berretta M et al. Resveratrol in Cancer Patients: From Bench to Bedside. Int J Mol Sci. 2020 Apr; 21(8): 2945.
51. Tomé-Carneiro et al. Grape Resveratrol Increases Serum Adiponectin and Downregulates Inflammatory Genes in Peripheral Blood Mononuclear Cells: A Triple-Blind, Placebo-Controlled, One-Year Clinical Trial in Patients with Stable Coronary Artery Disease. Cardiovascular Drugs and Therapy 27, nr. 1 (February 2013): 37–48.
52. Barger et al. A Low Dose of Dietary Resveratrol Partially Mimics Caloric Restriction and Retards Aging Parameters in Mice. PLoS ONE 3(6): 2008.
53. Guthrie A R et al. Effects of resveratrol on drug‐ and carcinogen‐metabolizing enzymes, implications for cancer prevention, 2017 https://doi.org/10.1002/prp2.294.
54. Sevki A et al. Modulatory Effects of Resveratrol on Liver, Kidney and Lung Total GST, GST Mu, NQO1 and CYP2B4, CYP2E1 and CYP3A Associated Enzyme Activities. Drug Metabolism Reviews, May 2009
55. https://coronalongplein.nl/informatie/hoe-verloopt-het-herstel
56. Berman A Y et al. The therapeutic potential of resveratrol: a review of clinical trials, NPJ Precis Oncol. 2017;1:35.
57. Quadros Gomes B et al. Neuroprotective Mechanisms of Resveratrol in Alzheimer’s Disease: Role of SIRT1. Oxidative Medicine and Cellular Longevity. Volume 2018.
58. Gianchecchi E, Fierabracci A. Insights on the Effects of Resveratrol and Some of Its Derivatives in Cancer and Autoimmunity: A Molecule with a Dual Activity, Antioxidants 2020, 9(2), 91.
59.Espinoza J L et al. The Repeated Administration of Resveratrol Has Measurable Effects on Circulating T-Cell Subsets in Humans. Oxidative Medicine and Cellular Longevity. Volume 2017.
60. Malaguarnera L, Influence of Resveratrol on the Immune Response. Nutrients. April 2019.11(5):946.
61. AbdelMassih A et al. Hypoxia-inducible factor (HIF): The link between obesity and COVID-19., Med. 2020 Dec 30:100317.
62. Xiao Meng et al. Health Benefits and Molecular Mechanisms of Resveratrol. Foods. 2020 Mar; 9(3): 340.
63. Singh A P et al. Health benefits of resveratrol: Evidence from clinical studies. Med Res Rev. 2019 Sep;39(5):1851-1891.
64. Detampel P et al. Drug interaction potential of resveratrol. Drug Metab Rev. 2012;44(3):253-265.
65. Baur Joseph et Sinclair David. Therapeutic potential of resveratrol. Biological Mechanisms of Aging, Harvard University, 2006.
66. Tse-Yin Huang et al. Resveratrol stereoselectively affected (±)warfarin pharmacokinetics and enhanced the anticoagulation effect. Scientific Reports. Sept. 2020, 10(1):15910.
67. Darby J R T et al. Systematic review: Impact of resveratrol exposure during pregnancy on maternal and fetal outcomes in animal models of human pregnancy complications-Are we ready for the clinic? Pharmacol Res. 2019 Jun;144:264-278.
68. Salehi P et al. Resveratrol: a Double-Edged Sword, Biomedicines 2018, 6(3), 91c.
69. Filardo S et al. Therapeutic potential of resveratrol against emerging respiratory viral infections. Pharmacol Ther. 2020 Oct;214:107613.
70. Galiniak S et al. Health benefits of resveratrol administration. Acta Biochim Pol. 2019 Feb 28;66(1):13-21.
71. Okamoto et al. Adiponectin: a key adipocytokine in metabolic syndrome. Clinical science 2006
72. Martinez MA. Compounds with Therapeutic Potential against Novel Respiratory 2019 Coronavirus. Antimicrob Agents Chemother. 2020 Apr 21;64(5):e00399-20.
73. Nascimento Junior JAC et al. SARS, MERS and SARS-CoV-2 (COVID-19) treatment: a patent review, Expert Opin Ther Pat., 2020 Aug;30(8):567-579.
74. Marinella MA. Indomethacin and resveratrol as potential treatment adjuncts for SARS-CoV-2/COVID-19. Int J Clin Pract. 2020 Sep;74(9):e13535.
75. Hooper PL. COVID-19 and heme oxygenase: novel insight into the disease and potential therapies, Cell Stress Chaperones. 2020 Sep;25(5):707-710.
76. Bousquet J et al. Nrf2-interacting nutrients and COVID-19: time for research to develop adaptation strategies, Clin Transl Allergy, 2020 Dec 3;10(1):58.
77. Giordo R et al. Therapeutic Potential of Resveratrol in COVID-19-Associated Hemostatic Disorders. Molecules, 2021 Feb 6;26(4):856.
79. Wahedi HM et al. Stilbene-based natural compounds as promising drug candidates against COVID-19. J Biomol Struct Dyn., 2020 May 12:1-10.
80. Hoang T. An approach of fatty acids and resveratrol in the prevention of COVID-19 severity. Phytother Res. 2020 Nov 17:10.1002/ptr.6956.
81. Ranjbar A et al. Molecular modelling of the antiviral action of Resveratrol derivatives against the activity of two novel SARS CoV-2 and 2019-nCoV receptors. Eur Rev Med Pharmacol Sci. 2020 Jul;24(14):7834-7844.
82. Limanaqi F et al. Cell Clearing Systems as Targets of Polyphenols in Viral Infections. Antioxidants (Basel)., 2020 Nov 10;9(11):1105.
83. Rege S D et al. Neuroprotective effects of resveratrol in Alzheimer disease pathology. Front Aging Neurosci. 2014; 6: 218.