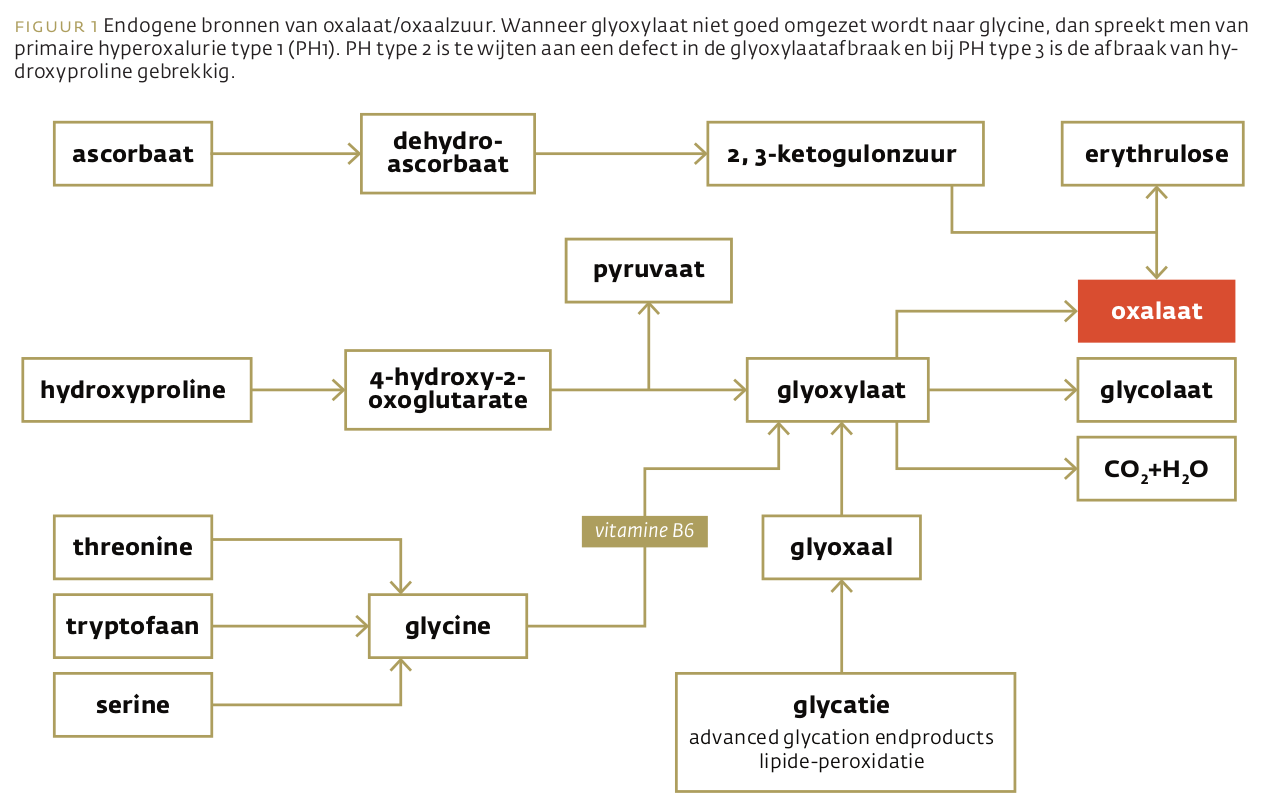
Oxalaat is een antinutriënt en een afvalstof van het metabolisme. Het grootste gevaar dat deze stof vormt, zijn nierstenen. Oxalaatrijke voeding, calcium en darmbacteriën bepalen samen het lot van oxalaat uit voeding, terwijl het metabolisme van aminozuren en ascorbaat ook hun steentje bijdraagt aan de uitscheiding van oxalaat. Hoe evident het ook lijkt, oxalaatrestrictie is nog steeds geen evidence-based behandeling.
Beste bezoeker, u heeft geen toegang.
Enkel (web)abonnees hebben toegang tot tijdschriftartikelen. Het webabonnement is nog in de maak.
U kunt zich wel alvast (gratis) registreren en tal van andere webartikelen raadplegen!
Auteur
Verschenen in
Referenties
Konstantynowicz J, Porowski T, Zoch-Zwierz W, et al. A potential pathogenic role of oxalate in autism. Eur J Paediatr Neurol. 2012;16(5):485-491. doi:10.1016/j.ejpn.2011.08.004
Perrotta I, Perri E. Ultrastructural, Elemental and Mineralogical Analysis of Vascular Calcification in Atherosclerosis. Microsc Microanal. 2017;23(5):1030-1039. doi:10.1017/S1431927617012533
Mitchell T, Kumar P, Reddy T et al. Dietary oxalate and kidney stone formation. Am J Physiol Renal Physiol. 2019 Mar 1;316(3):F409-F413. doi: 10.1152/ajprenal.00373.2018. Epub 2018 Dec 19. PMID: 30566003; PMCID: PMC6459305.
Holmes RP, Goodman HO, Assimos DG. Contribution of dietary oxalate to urinary oxalate excretion. Kidney Int. 2001;59(1):270-276. doi:10.1046/j.1523-1755.2001.00488.x
Robertson WG. Dietary recommendations and treatment of patients with recurrent idiopathic calcium stone disease. Urolithiasis. 2016; 44(1):9-26 doi:10.1007/s00240-015-0849-2
Schwen ZR, Riley JM, Shilo Y, Averch TD. Dietary management of idiopathic hyperoxaluria and the influence of patient characteristics and compliance. Urology. 2013; 82(6):1220-5 doi:10.1016/j.urology.2013.08.002
Noori N, Honarkar E, Goldfarb DS et al. Urinary lithogenic risk profile in recurrent stone formers with hyperoxaluria: a randomized controlled trial comparing DASH (Dietary Approaches to Stop Hypertension)-style and low-oxalate diets. Am J Kidney Dis. 2014; 63(3):456-63 doi:10.1053/j.ajkd.2013.11.022
Zimmermann DJ, Hesse A, von Unruh GE. Influence of a high-oxalate diet on intestinal oxalate absorption. World J Urol. 2005;23(5):324-329. doi:10.1007/s00345-005-0028-0
Lange JN, Wood KD, Mufarrij PW et al. The impact of dietary calcium and oxalate ratios on stone risk. Urology. 2012; 79(6):1226-9 doi:10.1016/j.urology.2012.01.053
Hess B, Jost C, Zipperle L, Takkinen R, Jaeger P. High-calcium intake abolishes hyperoxaluria and reduces urinary crystallization during a 20-fold normal oxalate load in humans. Nephrol Dial Transplant. 1998;13(9):2241-2247. doi:10.1093/ndt/13.9.2241
Matsumoto ED, Heller HJ, Adams-Huet B, Brinkley LJ, Pak CY, Pearle MS. Effect of high and low calcium diets on stone forming risk during liberal oxalate intake. J Urol. 2006;176(1):132-136. doi:10.1016/S0022-5347(06)00565-9
von Unruh GE, Voss S, Sauerbruch T, Hesse A. Dependence of oxalate absorption on the daily calcium intake. J Am Soc Nephrol. 2004; 15(6):1567-73 doi:10.1097/01.asn.0000127864.26968.7f
Eisner BH, Sheth S, Dretler SP et al. High dietary magnesium intake decreases hyperoxaluria in patients with nephrolithiasis. Urology. 2012; 80(4):780-3 doi:10.1016/j.urology.2012.06.033
Tavasoli S, Taheri M, Taheri F, Basiri A, Bagheri Amiri F. Evaluating the associations between urinary excretion of magnesium and that of other components in calcium stone-forming patients. Int Urol Nephrol. 2019;51(2):279-284. doi:10.1007/s11255-018-2036-1
Nouvenne A, Meschi T, Prati B, et al. Effects of a low-salt diet on idiopathic hypercalciuria in calcium-oxalate stone formers: a 3-mo randomized controlled trial. Am J Clin Nutr. 2010;91(3):565-570. doi:10.3945/ajcn.2009.28614
Ticinesi A, Nouvenne A, Chiussi G et al. Calcium Oxalate Nephrolithiasis and Gut Microbiota: Not just a Gut-Kidney Axis. A Nutritional Perspective. Nutrients. 2020; 12(2) doi:10.3390/nu12020548
Hatch M, Cornelius J, Allison M, Sidhu H, Peck A, Freel RW. Oxalobacter sp. reduces urinary oxalate excretion by promoting enteric oxalate secretion. Kidney Int. 2006;69(4):691-698. doi:10.1038/sj.ki.5000162
Lieske JC, Tremaine WJ, De Simone C, et al. Diet, but not oral probiotics, effectively reduces urinary oxalate excretion and calcium oxalate supersaturation. Kidney Int. 2010;78(11):1178-1185. doi:10.1038/ki.2010.310
Hoppe B, Niaudet P, Salomon R, et al. A randomised Phase I/II trial to evaluate the efficacy and safety of orally administered Oxalobacter formigenes to treat primary hyperoxaluria. Pediatr Nephrol. 2017;32(5):781-790. doi:10.1007/s00467-016-3553-8p
Hoppe B, Beck B, Gatter N, et al. Oxalobacter formigenes: a potential tool for the treatment of primary hyperoxaluria type 1. Kidney Int. 2006;70(7):1305-1311. doi:10.1038/sj.ki.5001707p
Shoag J, Tasian GE, Goldfarb DS, Eisner BH. The new epidemiology of nephrolithiasis. Adv Chronic Kidney Dis. 2015; 22(4):273-8 doi:10.1053/j.ackd.2015.04.004
Sakhaee K. Unraveling the mechanisms of obesity-induced hyperoxaluria. Kidney Int. 2018; 93(5):1038-1040 doi:10.1016/j.kint.2018.01.012
Amin R, Asplin J, Jung D, et al. Reduced active transcellular intestinal oxalate secretion contributes to the pathogenesis of obesity-associated hyperoxaluria. Kidney Int. 2018;93(5):1098-1107. doi:10.1016/j.kint.2017.11.011
Lange JN, Wood KD, Knight J et al. Glyoxal formation and its role in endogenous oxalate synthesis. Adv Urol. 2012; 2012:819202 doi:10.1155/2012/819202
Aydin H, Yencilek F, Erihan IB, Okan B, Sarica K. Increased 10-year cardiovascular disease and mortality risk scores in asymptomatic patients with calcium oxalate urolithiasis. Urol Res. 2011;39(6):451-458. doi:10.1007/s00240-011-0383-9
Efe O, Verma A, Waikar SS. Urinary oxalate as a potential mediator of kidney disease in diabetes mellitus and obesity. Curr Opin Nephrol Hypertens. 2019 Jul;28(4):316-320. doi: 10.1097/MNH.0000000000000515
Ermer T, Eckardt KU, Aronson PS, Knauf F. Oxalate, inflammasome, and progression of kidney disease. Curr Opin Nephrol Hypertens. 2016;25(4):363-371. doi:10.1097/MNH.0000000000000229
Noonan SC, Savage GP. Oxalate content of foods and its effect on humans. Asia Pac J Clin Nutr. 1999; 8(1):64-74
Liebman M, Al-Wahsh IA. Probiotics and other key determinants of dietary oxalate absorption. Adv Nutr. 2011; 2(3):254-60 doi:10.3945/an.111.000414
Smith CM, Marks AD, Lieberman MA. Marks' Basic Medical Biochemistry: A Clinical Approach, 2nd Edition, 2004, Williams and Wilkins (ISBN: 0-7817-2145-8)
Bender DA. Nutritional Biochemistry of the Vitamins. Cambridge University Press; 2 edition (October 29, 2009)
Brody T. Nutritional Biochemistry. Academic Press; 2 edition (December 21, 1998)
Knight J, Madduma-Liyanage K, Mobley JA et al. Ascorbic acid intake and oxalate synthesis. Urolithiasis. 2016; 44(4):289-97 doi:10.1007/s00240-016-0868-7
Akiduki S, Ito H, Morishita K, Kamimura A. A single-blind, parallel trial of L-hydroxyproline in healthy adult subjects. Urolithiasis. 2015 Jun;43(3):289-92. doi: 10.1007/s00240-015-0765-5. Epub 2015 Apr 1. PMID: 25827754; PMCID: PMC4436679.
Knight J, Jiang J, Assimos DG, Holmes RP. Hydroxyproline ingestion and urinary oxalate and glycolate excretion. Kidney Int. 2006;70(11):1929-1934. doi:10.1038/sj.ki.5001906p
Holmes RP, Kennedy M. Estimation of the oxalate content of foods and daily oxalate intake. Kidney Int. 2000; 57(4):1662-7 doi:10.1046/j.1523-1755.2000.00010.x
Attalla K, De S, Monga M. Oxalate content of food: a tangled web. Urology. 2014; 84(3):555-60 doi:10.1016/j.urology.2014.03.053
https://regepi.bwh.harvard.edu/health/Oxalate/files/Oxalate%20Content%20...
Chen K, Chen D, Lan C, et al. Does green tea consumption increase urinary oxalate excretion? Results of a prospective trial in healthy men. Int Urol Nephrol. 2018;50(1):29-33. doi:10.1007/s11255-017-1720-x
Shu X, Cai H, Xiang YB, et al. Green tea intake and risk of incident kidney stones: Prospective cohort studies in middle-aged and elderly Chinese individuals. Int J Urol. 2019;26(2):241-246. doi:10.1111/iju.13849
Zeng X, Xi Y, Jiang W. Protective roles of flavonoids and flavonoid-rich plant extracts against urolithiasis: A review. Crit Rev Food Sci Nutr. 2019;59(13):2125-2135. doi:10.1080/10408398.2018.1439880
Siener R, López-Mesas M, Valiente M, Blanco F. Determination of Oxalate Content in Herbal Remedies and Dietary Supplements Based on Plant Extracts. J Med Food. 2016;19(2):205-210. doi:10.1089/jmf.2015.0068
Ghosh Das S, Savage GP. Total and soluble oxalate content of some Indian spices. Plant Foods Hum Nutr. 2012;67(2):186-190. doi:10.1007/s11130-012-0278-0
Tang M, Larson-Meyer DE, Liebman M. Effect of cinnamon and turmeric on urinary oxalate excretion, plasma lipids, and plasma glucose in healthy subjects. Am J Clin Nutr. 2008;87(5):1262-1267. doi:10.1093/ajcn/87.5.1262
Knight J, Easter LH, Neiberg R et al. Increased protein intake on controlled oxalate diets does not increase urinary oxalate excretion. Urol Res. 2009; 37(2):63-8 doi:10.1007/s00240-009-0170-z
Ghodasara J, Pawar A, Deshmukh C, Kuchekar B. Inhibitory effect of rutin and curcumin on experimentally-induced calcium oxalate urolithiasis in rats. Pharmacognosy Res. 2010;2(6):388-392. doi:10.4103/0974-8490.75462
Espino-Grosso P, Monsour C, Canales BK. The Effect of Calcium and Vitamin B6 Supplementation on Oxalate Excretion in a Rodent Gastric Bypass Model of Enteric Hyperoxaluria. Urology. 2019;124:310.e9-310.e14. doi:10.1016/j.urology.2018.06.061
Fargue S, Milliner DS, Knight J et al. Hydroxyproline Metabolism and Oxalate Synthesis in Primary Hyperoxaluria. J Am Soc Nephrol. 2018; 29(6):1615-1623 doi:10.1681/ASN.2017040390