De lever is een orgaan met een enorm regeneratief vermogen.
Iets wat al sedert de Oudheid tot de verbeelding spreekt. Denk
aan het verhaal uit de Griekse mythologie, de aan een rots
geketende Prometheus bij wie dagelijks een stuk van zijn lever
opgevreten werd door de adelaar van Zeus. Door de grote
regeneratiecapaciteit groeide zijn lever echter weer iedere dag
aan, zodat de kwelling eeuwig kon doorgaan.1,2
Beste bezoeker, u heeft geen toegang.
Enkel (web)abonnees hebben toegang tot tijdschriftartikelen. Het webabonnement is nog in de maak.
U kunt zich wel alvast (gratis) registreren en tal van andere webartikelen raadplegen!
Auteur
Verschenen in
Referenties
Power C, Rasko JE. Whither prometheus' liver? Greek myth and the science of regeneration. Ann Intern Med. 2008 Sep 16;149(6):421-6.
Tiniakos DG, Kandilis A, Geller SA. Tityus: a forgotten myth of liver regeneration. J Hepatol. 2010 Aug;53(2):357-61.
Pruimboom L. De lever/pancreas/resistenties binnen de klinische PNI. Bachelor cursus cPNI, 2e jaar 2011.
Gordillo M, Evans T, Gouon-Evans V. Orchestrating liver development. Development. 2015 Jun 15;142(12):2094-2108.
Rehman K, Iqbal MJ, Zahra N, Akash MS. Liver stem cells: from preface to advancements. Curr Stem Cell Res Ther. 2014 Jan;9(1):10-21.
Fausto, N, Campbell JS, Riehle KJ. Liver regeneration. J. Hepatol. 2012, 57, 692–694.
Thorgeirsson SS. Hepatic stem cells in liver regeneration. FASEB J. 1996, 10, 1249–1256.
Tanimizu N, Mitaka T. Re-evaluation of liver stem/progenitor cells. Organogenesis. 2014 Apr-Jun;10(2):208-15.
Muskiet FAJ, Muskiet MHA. Chronische systemische lagegraadontsteking: de opmaat voor het insulineresistentiesyndroom en sequelae. AT&A 2012; 1:10-16.
Kirpich IA, Marsano LS, McClain CJ. Gut-liver axis, nutrition, and non-alcoholic fatty liver disease. Clin Biochem. 2015 Jul 4. pii: S0009-9120(15)00261-1.
Martinon F, Mayor et al. The inflammasomes are the guardians of the body. Annu Rev Immunol 2009; 27:229-65.
Lin XJ, Yang J, Chen XB, Zhang M, Xu MQ. The critical value of remnant liver volume-to-body weight ratio to estimate posthepatectomy liver failure in cirrhotic patients. J Surg Res. 2014 May 15;188(2):489-95.
Lafaro K et al. Defining Post Hepatectomy Liver Insufficiency: Where do We stand? J Gastrointest Surg. 2015 Jun 11. [Epub ahead of print]
Manti S et al. Nonalcoholic Fatty liver disease/non-alcoholic steatohepatitis in childhood: endocrine-metabolic "mal-programming". Hepat Mon. 2014 May 1;14(5):e17641.
Fusillo S, Rudolph B. Nonalcoholic fatty liver disease. Pediatr Rev. 2015 May;36(5):198-205
Ahmed M et al. Non-alcoholic fatty liver disease in 2015. World J Hepatol 2015 Jun 18;7(11):1450-9.
Sharma M et al. The Riddle of Nonalcoholic Fatty Liver Disease: Progression From Nonalcoholic Fatty Liver to Nonalcoholic Steatohepatitis. J Clin Exp Hepatol. 2015 Jun;5(2):147-58.
Rinella ME. Nonalcoholic fatty liver disease: a systematic review. JAMA. 2015 Jun 9;313(22):2263-73
Hassan K, Bhalla V, El Regal ME, A-Kader HH. Nonalcoholic fatty liver disease: a comprehensive review of a growing epidemic. World J Gastroenterol. 2014; 20(34):12082-101.
Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015 Apr;62(1 Suppl):S47-64.
Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011 Aug;34(3):274-85.
Pár G, Horváth G, Pár A. Non-alcoholic fatty liver disease and steatohepatitis. Orv Hetil. 2013 Jul 21;154(29):1124-34.
Pasarín M et al. Insulin resistance and liver microcirculation in a rat model of early NAFLD. J Hepatol. 2011 Nov;55(5):1095-102.
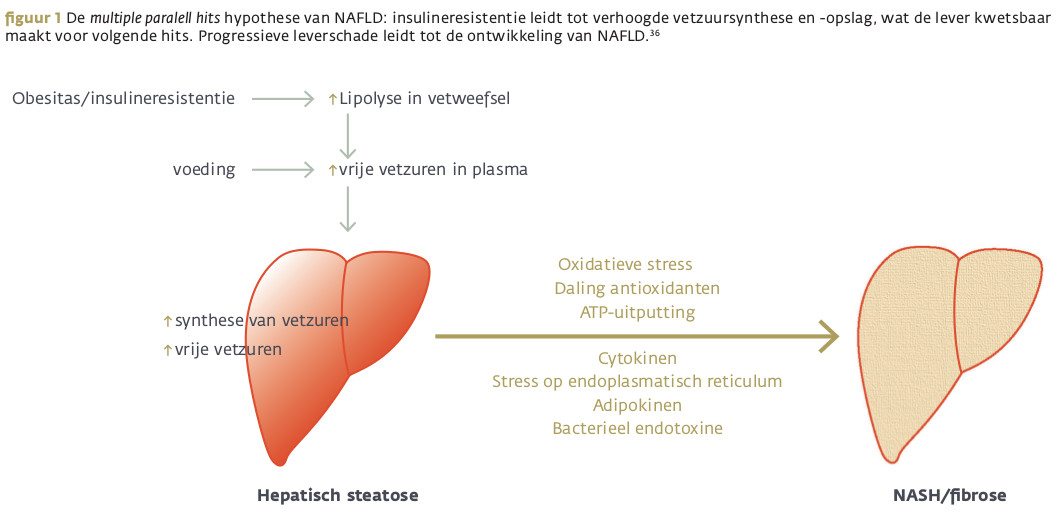
Pasarín M et al. Sinusoidal endothelial dysfunction precedes inflammation and fibrosis in a model of NAFLD. PLoS One. 2012;7(4):e32785.
Angulo P, Machado MV, Diehl AM. Fibrosis in nonalcoholic Fatty liver disease: mechanisms and clinical implications. Semin Liver Dis. 2015 May;35(2):132-45
Nobili V et al. Altered gut-liver axis and hepatic adiponectin expression in OSAS: novel mediators of liver injury in paediatric non-alcoholic fatty liver. Thorax. 2015 Jun 11. pii: thoraxjnl-2015-206782.
doi: 10.1556/OH.2009.28749.
Hagymási K, Reismann P, Rácz K, Tulassay Z. Role of the endocrine system in the pathogenesis of non-alcoholic fatty liver disease. Orv Hetil. 2009 Nov 29;150(48):2173-81.
Conigliaro A, Brenner DA, Kisseleva T. Hepatic progenitors for liver disease: current position. Stem Cells Cloning. 2010 Feb 25;3:39-47.
Ide T et al. Cross-talk between peroxisome proliferator-activated receptor (PPAR) alpha and liver X receptor (LXR) in nutritional regulation of fatty acid metabolism. II. LXRs suppress lipid degradation gene promoters through inhibition of PPAR signaling. Mol Endocrinol. 2003 Jul;17(7):1255-67
Bosma-den Boer, van Wetten ML, Pruimboom L. Chronic inflammatory diseases are stimulated by current lifestyle: … Nutr & metabol 2012; 9:32.
Pruimboom L, Nys M. Een nieuw behandelingsmodel voor niet-infectieuze ziekten. AT&A 2013; 4: 10-15.
Bismuth M et al. Hepatic encephalopathy: from pathophysiology to therapeutic management. Eur J Gastroenterol Hepatol. 2011 Jan;23(1):8-22.
Miletić V et al. Parkinsonian syndrome and ataxia as a presenting finding of acquired hepatocerebral degeneration. Metab Brain Dis. 2014 Mar;29(1):207-9.
Romeiro FG et al. Acquired hepatocerebral degeneration and hepatic encephalopathy: correlations and variety of clinical presentations in overt and subclinical liver disease. Arq Neuropsiquiatr. 2011 Jun;69(3):496-501.
Nassir F, Ibdah JA. Role of Mitochondria in Nonalcoholic Fatty Liver Disease. Int J Mol Sci. 2014; 15(5): 8713–8742.
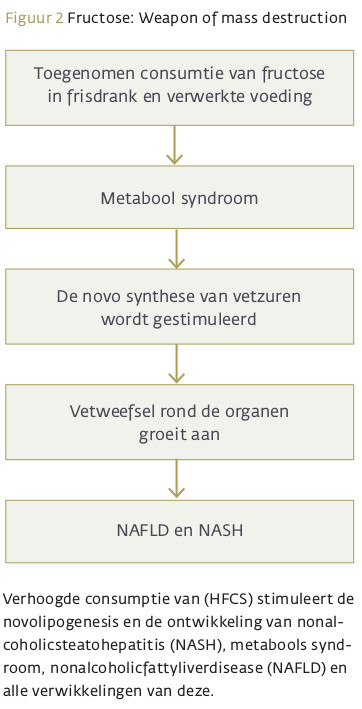
Basaranoglu , Basaranoglu G, Bugianesi E. Carbohydrate intake and nonalcoholic fatty liver disease: fructose as a weapon of mass destruction. Hepatobiliary Surg Nutr. 2015 Apr;4(2):109-16
Collison KS. Diabetes of the liver: the link between nonalcoholic fatty liver disease and HFCS-55. Obesity (Silver Spring). 2009 Nov;17(11):2003-13.
Tetri LH et al. Severe NAFLD with hepatic necroinflammatory changes in mice fed trans fats and a high-fructose corn syrup equivalent. Am J Physiol Gastrointest Liver Physiol. 2008 Nov;295(5):G987-95.
Basaranoglu M, Basaranoglu G, Sabuncu T, Sentürk H. Fructose as a key player in the development of fatty liver disease. World J Gastroenterol. 2013 Feb 28;19(8):1166-72.
Vos MB, Lavine JE. Dietary fructose in nonalcoholic fatty liver disease. Hepatology. 2013 Jun;57(6):2525-31.
Abdelmalek M et al. Higher dietary fructose is associated with impaired hepatic adenosine triphosphate homeostasis in obese individuals with type 2 diabetes. Hepatology. 2012 Sep;56(3):952-60.
Bray GA, Popkin BM. Calorie-sweetened beverages and fructose: what have we learned 10 years later. Pediatr Obes. 2013 Aug;8(4):242-8.
Carbohydrate metabolism. http://www.medbio.info/Horn/PDF%20files/carbohydrate_metabolism.pdf
http://www.zoelho.com/ZoelhoNL/Publish/index.htm#t=Basiselementen%2FVoed...
Nseir W, Nassar F, Assy N. Soft drinks consumption and nonalcoholic fatty liver disease. World J Gastroenterol. 2010 Jun 7;16(21):2579-88.
Abid A, Taha O, Nseir W, Farah R, Grosovski M, Assy N. Soft drink consumption is associated with fatty liver disease independent of metabolic syndrome. J Hepatol. 2009 Nov;51(5):918-24.
Moore JB, Gunn PJ, Fielding BA. The role of dietary sugars and de novo lipogenesis in non-alcoholic fatty liver disease. Nutrients. 2014 Dec 10;6(12):5679-703.
Bray GA, Popkin B. Dietary sugar and body weight: have we reached a crisis in the epidemic of obesity and diabetes? Diabetes Care. 2014 Apr;37(4):950-6.
Yoshida M et al. Surrogate markers of insulin resistance are associated with consumption of sugar-sweetened drinks and fruit juice in middle and older-aged adults. J Nutr. 2007 Sep;137(9):2121-7.
Shih MH et al. Association between serum uric acid and nonalcoholic fatty liver disease in the US population. J Formos Med Assoc. 2015 Apr;114(4):314-20.
Liu PJ, Ma F, Lou HP, Zhu YN, Chen Y. Relationship between serum uric acid levels and hepatic steatosis in non-obese postmenopausal women. Climacteric. 2014 Dec;17(6):692-9.
Nobili V et al. Altered gut-liver axis and hepatic adiponectin expression in OSAS: novel mediators of liver injury in paediatric non-alcoholic fatty liver. Thorax. 2015 Jun 11. pii: thoraxjnl-2015-206782.
Batt C et al. Sugar-sweetened beverage consumption: a risk factor for prevalent gout with SLC2A9 genotype-specific effects on serum urate and risk of gout. Ann Rheum Dis. 2014 Dec;73(12):2101-6.
Merriman TR, Dalbeth N, Johnson RJ. Sugar-sweetened beverages, urate, gout and genetic interaction. Pac Health Dialog. 2014 Mar;20(1):31-8.
Murphy R et al. Sugar Sweetened Beverage Consumption among Adults with Gout or Type 2 Diabetes. PLoS One. 2015 May 15;10(5):e0125543.
Abeles AM, Park JY et al. Update on gout: pathofysiology and potential treatments. Curr Pain Headache Rep 2007; 11(6):440-6.
Cronstein NB. Gout: forgotten therapy for a common disease. Curr rheumatol Rep 2005; 7(1):1-2.
Cronstein NB, Terkeltaub R. The inflammatory proces of gout en its treatment. Atrtritis rest her 2006; 8S1:53.
Gasse P, Riteau et al. Uric acid is a danger signal activating NALP3 inflammasome in lung injury inflammation and fibrosis. Am J Respir Crit Care med 2009; 179(10):903-13.
Pruimboom L, Nys M. Een nieuw behandelingsmodel voor niet-infectieuze ziekten. AT&A 2013; 4: 10-15.
Li DY, Yang M, Edwards S, Ye SQ. Nonalcoholic fatty liver disease: for better or worse, blame the gut microbiota? JPEN J Parenter Enteral Nutr. 2013 Nov;37(6):787-93.
Cao ZJ et al. Research advances in the gut microbiota and inflammation in obesity. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2013 Aug;35(4):462-5.
Morales P, Brignardello J, Gotteland M. The association of intestinal microbiota with obesity. Rev Med Chil. 2010;138(8):1020-7.
Ferolla SM, Armiliato GN, Couto CA, Ferrari TC. The role of intestinal bacteria overgrowth in obesity-related nonalcoholic fatty liver disease. Nutrients. 2014 Dec 3;6(12):5583-99.
Frazier TH, DiBaise JK, McClain CJ. Gut microbiota, intestinal permeability, obesity-induced inflammation, and liver injury. JPEN J Parenter Enteral Nutr 2011 Sep;35(5 Suppl):14S-20S.
Malaguarnera G, Giordano M, Nunnari G, Bertino G, Malaguarnera M. Gut microbiota in alcoholic liver disease: pathogenetic role and therapeutic perspectives. World J Gastroenterol. 2014 Nov 28;20(44):16639-48.
Michail S et al. Altered gut microbial energy and metabolism in children with non-alcoholic fatty liver disease. FEMS Microbiol Ecol. 2015 Feb;91(2):1-9.
Vajro P, Paolella G, Fasano A. Microbiota and gut-liver axis: their influences on obesity and obesity-related liver disease. J Pediatr Gastroenterol Nutr. 2013 May;56(5):461-8.
Zhu L et al. Hepatology. 2013 Feb;57(2):601-9. Characterization of gut microbiomes in nonalcoholic steatohepatitis (NASH) patients: a connection between endogenous alcohol and NASH.
Tiegs G, Lohse AW. Immune tolerance: what is unique about the liver. J Autoimmun. 2010 Feb;34(1):1-6.
Knolle PA, Gerken G. Local control of the immune response in the liver. Immunol Rev. 2000 Apr;174:21-34.
Neumann K et al. Liver sinusoidal endothelial cells induce immunosuppressive IL-10-producing Th1 cells via the Notch pathway. Eur J Immunol. 2015 Jul;45(7):2008-16.
Kmieć Z. Cooperation of liver cells in health and disease. Adv Anat Embryol Cell Biol. 2001;161:III-XIII, 1-151.
Williams R. Review article: bacterial flora and pathogenesis in hepatic encephalopathy. Aliment Pharmacol Ther. 2007 Feb;25 Suppl 1:17-22.
Korek E, Krauss H. Novel adipokines: their potential role in the pathogenesis of obesity and metabolic disorders. Postepy Hig Med Dosw (Online). 2015 Jan 2;69(0):799-810.
Vienberg SG, Kleinridders A, Suzuki R, Kahn CR. Differential effects of angiopoietin-like 4 in brain and muscle on regulation of lipoprotein lipase activity. Mol Metab. 2014 Nov 13;4(2):144-50.
Kersten S. Regulation of lipid metabolism via angiopoietin-like proteins. Biochem Soc Trans. 2005 Nov;33(Pt 5):1059-62.
Mandard S et al. The fasting-induced adipose factor/angiopoietin-like protein 4 is physically associated with lipoproteins and governs plasma lipid levels and adiposity. J Biol Chem. 2006 Jan 13;281(2):934-44.
Mattijssen F, Kersten S. Regulation of triglyceride metabolism by Angiopoietin-like proteins. Biochim Biophys Acta. 2012;1821(5):782-9.
Plekhanov AN. Certain aspects of therapy of acute hepatic insufficiency. Klin Med (Mosk). 2013;91(9):16-21.
Dantoft TM, Andersson L, Nordin S, Skovbjerg S. Chemical Intolerance. Curr Rheumatol Rev. 2015;11(2):167-84.
Sparks PJ et al. Multiple chemical sensitivity syndrome: a clinical perspective. I. Case definition, theories of pathogenesis, and research needs. J Occup Med. 1994 Jul;36(7):718-30.
Sorg BA. Multiple chemical sensitivity: potential role for neural sensitization. Crit Rev Neurobiol. 1999;13(3):283-316.
Regal Ramos RJ. Can we rule out that fibromyalgia, chronic fatigue syndrome and multiple chemical sensitivity are psychosomatic diseases? Semergen. 2015 Jul 24. pii: S1138-3593(15)00169-0.
Lee WM. Acute liver failure. Semin Respir Crit Care Med. 2012 Feb;33(1):36-45.
Hug BL, Surber C, Bates DW. Use of hepatotoxic drugs in chronic liver disease. J Patient Saf. 2012 Jun;8(2):45-50.
Björnsson E. The natural history of drug-induced liver injury. Semin Liver Dis. 2009 Nov;29(4):357-63.
Rangnekar AS, Fontana RJ. An update on drug induced liver injury. Minerva Gastroenterol Dietol. 2011 Jun;57(2):213-29.
Chalasani N et al. Features and Outcomes of 899 Patients With Drug-Induced Liver Injury: The DILIN Prospective Study. Gastroenterology. 2015 Jun;148(7):1340-52.e7.
Molleston JP et al. Characteristics of idiosyncratic drug-induced liver injury in children: results from the DILIN prospective study. J Pediatr Gastroenterol Nutr. 2011 Aug;53(2):182-9.
Hug BL, Surber C, Bates DW. Use of hepatotoxic drugs in chronic liver disease. J Patient Saf. 2012 Jun;8(2):45-50.
Björnsson E. The natural history of drug-induced liver injury. Semin Liver Dis. 2009 Nov;29(4):357-63.
Rangnekar AS, Fontana RJ. An update on drug induced liver injury. Minerva Gastroenterol Dietol. 2011 Jun;57(2):213-29.
Chalasani N et al. Features and Outcomes of 899 Patients With Drug-Induced Liver Injury: The DILIN Prospective Study. Gastroenterology. 2015 Jun;148(7):1340-52.e7.
Jaeschke H. Acetaminophen: Dose-Dependent Drug Hepatotoxicity and Acute Liver Failure in Patients. Dig Dis. 2015;33(4):464-71.
Chun LJ, Tong MJ, Busuttil RW, Hiatt JR. Acetaminophen hepatotoxicity and acute liver failure. Clin Gastroenterol. 2009 Apr;43(4):342-9.
Molleston JP et al. Characteristics of idiosyncratic drug-induced liver injury in children: results from the DILIN prospective study. J Pediatr Gastroenterol Nutr. 2011 Aug;53(2):182-9.
Bunchorntavakul C, Reddy KR. Acetaminophen-related hepatotoxicity. Clin Liver Dis. 2013 Nov;17(4):587-607.
Tobwala S, Khayyat A, Fan W, Ercal N. Comparative evaluation of N-acetylcysteine and N-acetylcysteineamide in acetaminophen-induced hepatotoxicity in human hepatoma HepaRG cells. Exp Biol Med (Maywood). 2015 Feb;240(2):261-72.
Pruimboom L. Insulineresistentie: Van perifeer naar centraal niveau ‘Een pandemisch probleem’. ATA 12-2
Daib-Conquy M, Cavaillon JM. Stress molecules in sepsis and systemic inflammatory response syndrome. FEBS Letters 2007; 581:3723-33.
Tilg H, Moschen AR. Inflammatory Mechanisms in the Regulatio of Insulin Resistance. Mol Med 2008; 14(3-4):222-31.
Boutagy NE, McMillan RP, Frisard MI, Hulver MW. Metabolic endotoxemia with obesity: Is it real and is it relevant? Biochimie. 2015 Jun 29. pii: S0300-9084(15)00199-6.
Rai R, Saraswat VA, Dhiman RK. Gut microbiota: its role in hepatic encephalopathy. J Clin Exp Hepatol. 2015 Mar;5(Suppl 1):S29-36.
Wolf MJ et al. Metabolic Activation of Intrahepatic CD8 T Cells and NKT Cells Causes Nonalcoholic Steatohepatitis and Liver Cancer via Cross-Talk with Hepatocytes. Cancer Cell, 2014; 26 (4): 549
Wang H, Yin S. Natural killer T cells in liver injury, inflammation and cancer. Expert Rev Gastroenterol Hepatol. 2015 Jun 11:1-9. [Epub ahead of print]
Kang LI, Mars WM, Michalopoulos GK. Signals and cells involved in regulating liverregeneration. Cell 2012, 13, 1261–1292.
Siddiqui MS et al. Nonalcoholic Steatohepatitis (NASH) Is Associated with a Decline in Pancreatic Beta Cell (β-Cell) Function. Dig Dis Sci. 2015 Aug;60(8):2529-37.
Nys M. De pancreas, van conceptie tot levenseinde. AT&A 2014; 1:13-17.
Nys M. Spijsverteringsenzymen zijn miskend maar essentieel. AT&A 2012; 5:18-23.
Rehman K, Iqbal MJ, Zahra N, Akash MS. Liver stem cells: from preface to advancements. Curr Stem Cell Res Ther. 2014 Jan;9(1):10-21.
Kordes C, Sawitza I, Götze S, Häussinger D. Bile acids and stellate cells. Dig Dis. 2015;33(3):332-7.
Fan M, Wang X, Xu G, Yan Q, Huang W. Bile acid signaling and liver regeneration. Biochim Biophys Acta. 2015 Feb;1849(2):196-200.
Wenfeng Z et al. Kupffer cells: increasingly significant role in nonalcoholic fatty liver disease. Ann Hepatol. 2014 Sep-Oct;13(5):489-95.
Jourdainne V et al. The Bile Acid Receptor TGR5 and Liver Regeneration. Dig Dis. 2015;33(3):319-26.
Götze S, Schumacher EC, Kordes C, Häussinger D. Epigenetic Changes during Hepatic Stellate Cell Activation. PLoS One. 2015 Jun 12;10(6):e0128745.
Zeng W et al. Antioxidant treatment enhances human mesenchymal stem cell anti-stress ability and therapeutic efficacy in an acute liver failure model. Sci Rep. 2015; 5:11100.
Morales-González JA, Sánchez-Moreno C et al. What is Known Regarding the Participation of Factor Nrf-2 in Liver Regeneration? Cells. 2015 May 20;4(2):169-77.
Cretoiu SM, Popescu LM. Telocytes revisited. Biomol Concepts. 2014 Oct;5(5):353-69. (www.telocytes.com).
Bei Y, Wang F, Yang C, Xiao J. Telocytes in regenerative medicine. J Cell Mol Med. 2015 Jun 8. doi: 10.1111/jcmm.12594. [Epub ahead of print]
Morales-González JA, Sánchez-Moreno C et al. What is Known Regarding the Participation of Factor Nrf-2 in Liver Regeneration? Cells. 2015 May 20;4(2):169-77.
Shin SM, Yang JH, Ki SH. Role of the Nrf2-ARE pathway in liver diseases. Oxid. Med. Cell. Longev.2013; doi:10.1155/2013/763257.
Michalopoulos GK. Nrf2, not always friendly but perhaps misunderstood. Hepatology 2014; 60:461–463.
Beyer TA, Werner S et al. Impaired liver regeneration in Nrf2 knockout mice: Role of ROS-mediated insulin/IGF-1 resistance. EMBO J. 2008, 27, 212–223.
Nys M. Fytohormese. AT&A 2014; 5:26-33.