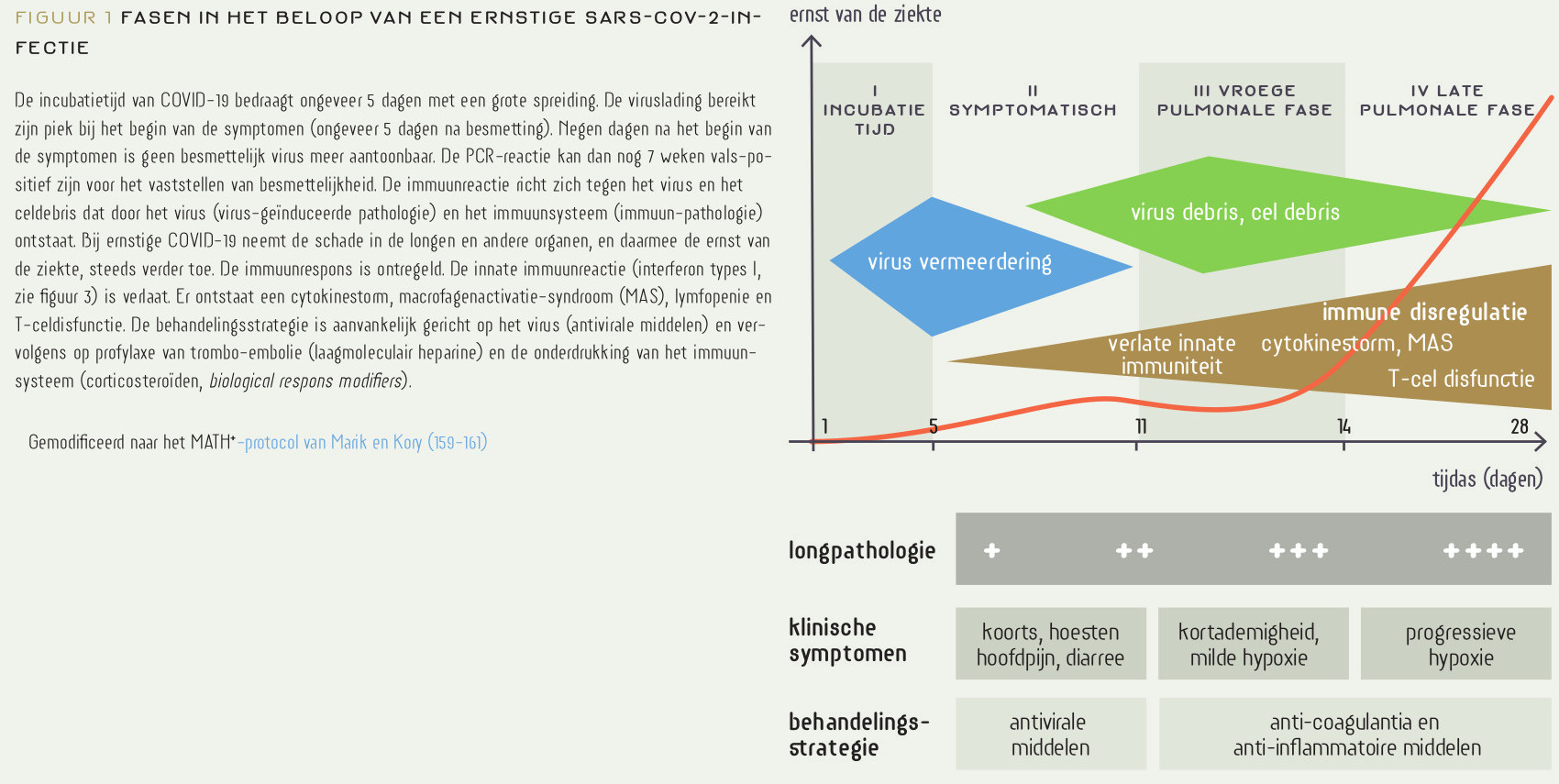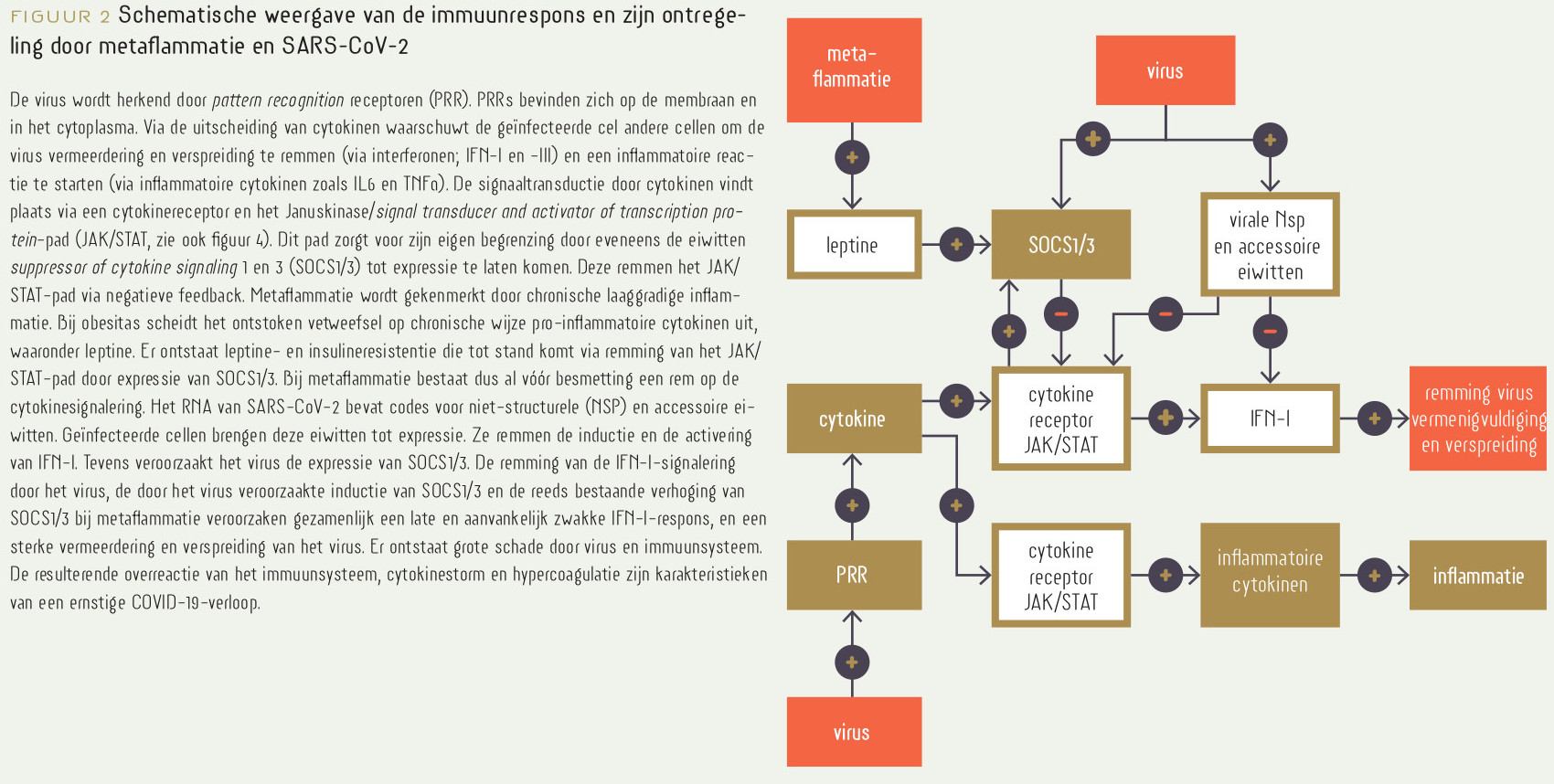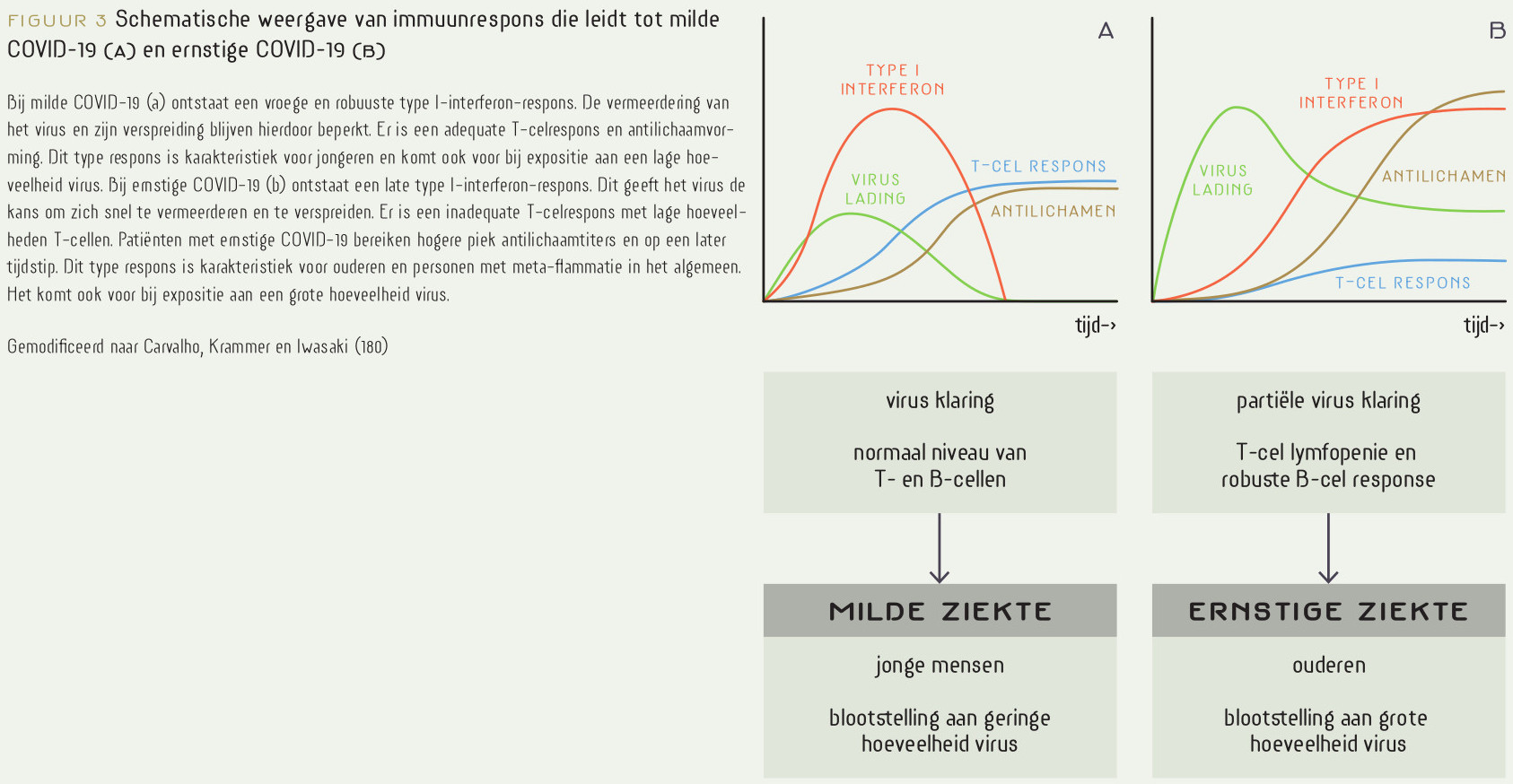
Coronavirus disease-2019 (COVID-19) wordt veroorzaakt door het severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Belangrijke risicofactoren voor ernstige COVID-19 zijn leeftijd, obesitas, mannelijk geslacht en obesitasgeassocieerde morbiditeit zoals hypertensie, diabetes mellitus type 2, hart-vaatziekte en chronische nierziekte. De gemeenschappelijke noemer is metaflammatie, een samentrekking van metabolisme en inflammatie. Indien een persoon met metaflammatie besmet raakt met SARS-CoV-2, wordt in eerste instantie geen toestemming verleend om een energieconsumerende en schadeveroorzakende immuunreactie te starten. Een vroege productie van interferonen type I blijft uit. Type I-interferonen hebben antivirale eigenschappen en voorkómen een snelle virusvermenigvuldiging en -verspreiding. Door de interferonsignalering te verstoren doet SARS-CoV-2 daar een forse schep bovenop. De bij metaflammatie heersende chronisch licht verhoogde spiegels van pro-inflammatoire cytokinen, leptine en insuline veroorzaken leptine- en insulineresistentie in (onder andere) het immuunsysteem. Verhoogde pro-inflammatoire cytokinen en leptine zijn bij obesitas afkomstig uit het ontstoken vetweefselcompartiment, drijven de leptine- en insulineresistentie, en de bijbehorende hyperleptinemie, hyperinsulinemie, hypertensie, hyperglycemie, hyperlipidemie en andere symptomen van het metabool syndroom. Mechanistisch wordt de leptineresistentie veroorzaakt door de inductie van suppressor of cytokine signaling 1 en 3 (SOCS1/3). Een consequentie is dat glucose niet kan worden opgenomen voor de activering van het immuunsysteem. SOCS1/3 wordt ook door het virus geïnduceerd. Door de late immuunreactie ontstaat grote schade door virus en immuunsysteem, dat vervolgens over-reageert. Er ontstaat een cytokinestorm, ernstige endotheelschade, hypercoagulatie en ernstige COVID-19. Het superponeren van een acute verstoring, zoals een SARS-CoV-2-infectie, op metaflammatie stelt de veerkracht sterk op de proef. Op lange termijn veroorzaakt metaflammatie de pathologie die we intussen goed kennen als de ‘typisch westerse’ ziekten die geassocieerd zijn met het metabool syndroom. Ernstige COVID-19 en andere ernstig verlopende infectieziekten kunnen daaraan als korte-termijnrisicofactoren worden toegevoegd. Voorkómen van besmetting, vaccinatie en verbetering van leefstijl zijn de beste preventieve maatregelen.
Beste bezoeker, u heeft geen toegang.
Enkel (web)abonnees hebben toegang tot tijdschriftartikelen. Het webabonnement is nog in de maak.
U kunt zich wel alvast (gratis) registreren en tal van andere webartikelen raadplegen!
Auteur
Verschenen in
Referenties
1. Oran DP, Topol EJ. The Proportion of SARS-CoV-2 Infections That Are Asymptomatic : A Systematic Review. Ann Intern Med. 2021 Jan 22:M20-6976. doi: 10.7326/M20-6976. Epub ahead of print. PMID: 33481642; PMCID: PMC7839426.
https://pubmed.ncbi.nlm.nih.gov/33481642/
2. Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA. 2020 Aug 25;324(8):782-793. doi: 10.1001/jama.2020.12839. PMID: 32648899.
https://pubmed.ncbi.nlm.nih.gov/32648899/
3. Ryan DH, Ravussin E, Heymsfield S. COVID 19 and the Patient with Obesity - The Editors Speak Out. Obesity (Silver Spring). 2020 May;28(5):847. doi: 10.1002/oby.22808. Epub 2020 Apr 1. PMID: 32237212; PMCID: PMC7228389.
https://pubmed.ncbi.nlm.nih.gov/32237212/
4. Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention. [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China]. Zhonghua Liu Xing Bing Xue Za Zhi. 2020 Feb 10;41(2):145-151. Chinese. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. PMID: 32064853.
https://pubmed.ncbi.nlm.nih.gov/32064853/
5. COVID-19 Data Explorer. Case fatality rate of the ongoing COVID-19 pandemic. Accessed 14 April 2021
https://ourworldindata.org/explorers/coronavirus-data-explorer?hideContr...
6. Cevik M, Kuppalli K, Kindrachuk J, Peiris M. Virology, transmission, and pathogenesis of SARS-CoV-2. BMJ. 2020 Oct 23;371:m3862. doi: 10.1136/bmj.m3862. PMID: 33097561.
https://pubmed.ncbi.nlm.nih.gov/33097561/
6a. Tang JW, Marr LC, Li Y, Dancer SJ. Covid-19 has redefined airborne transmission. BMJ. 2021 Apr 14;373:n913. doi: 10.1136/bmj.n913. PMID: 33853842.
https://pubmed.ncbi.nlm.nih.gov/33853842/
6b. Allen JG, Ibrahim AM. Indoor Air Changes and Potential Implications for SARS-CoV-2 Transmission. JAMA. 2021 Apr 16. doi: 10.1001/jama.2021.5053. Epub ahead of print. PMID: 33861316.
https://pubmed.ncbi.nlm.nih.gov/33861316/
7. Mauvais-Jarvis F. Aging, Male Sex, Obesity, and Metabolic Inflammation Create the Perfect Storm for COVID-19. Diabetes. 2020 Sep;69(9):1857-1863. doi: 10.2337/dbi19-0023. Epub 2020 Jul 15. PMID: 32669390; PMCID: PMC7458034.
https://pubmed.ncbi.nlm.nih.gov/32669390/
8. Gao F, Zheng KI, Wang XB, Sun QF, Pan KH, Wang TY, Chen YP, Targher G, Byrne CD, George J, Zheng MH. Obesity Is a Risk Factor for Greater COVID-19 Severity. Diabetes Care. 2020 Jul;43(7):e72-e74. doi: 10.2337/dc20-0682. Epub 2020 May 14. PMID: 32409499.
https://pubmed.ncbi.nlm.nih.gov/32409499/
9. Gao YD, Ding M, Dong X, Zhang JJ, Kursat Azkur A, Azkur D, Gan H, Sun YL, Fu W, Li W, Liang HL, Cao YY, Yan Q, Cao C, Gao HY, Brüggen MC, van de Veen W, Sokolowska M, Akdis M, Akdis CA. Risk factors for severe and critically ill COVID-19 patients: A review. Allergy. 2021 Feb;76(2):428-455. doi: 10.1111/all.14657. Epub 2020 Dec 4. PMID: 33185910.
https://pubmed.ncbi.nlm.nih.gov/33185910/
10. Mueller AL, McNamara MS, Sinclair DA. Why does COVID-19 disproportionately affect older people? Aging (Albany NY). 2020 May 29;12(10):9959-9981. doi: 10.18632/aging.103344. Epub 2020 May 29. PMID: 32470948; PMCID: PMC7288963.
https://pubmed.ncbi.nlm.nih.gov/32470948/
11. Sacco V, Rauch B, Gar C, Haschka S, Potzel AL, Kern-Matschilles S, Banning F, Benz I, Meisel M, Seissler J, Lechner A. Overweight/obesity as the potentially most important lifestyle factor associated with signs of pneumonia in COVID-19. PLoS One. 2020 Nov 18;15(11):e0237799. doi: 10.1371/journal.pone.0237799. PMID: 33206653; PMCID: PMC7673531.
https://pubmed.ncbi.nlm.nih.gov/33206653/
12. Mohammad S, Aziz R, Al Mahri S, Malik SS, Haji E, Khan AH, Khatlani TS, Bouchama A. Obesity and COVID-19: what makes obese host so vulnerable? Immun Ageing. 2021 Jan 4;18(1):1. doi: 10.1186/s12979-020-00212-x. PMID: 33390183; PMCID: PMC7779330.
https://pubmed.ncbi.nlm.nih.gov/33390183/
13. De Larochelambert Q, Marc A, Antero J, Le Bourg E, Toussaint JF. Covid-19 Mortality: A Matter of Vulnerability Among Nations Facing Limited Margins of Adaptation. Front Public Health. 2020 Nov 19;8:604339. doi: 10.3389/fpubh.2020.604339. PMID: 33330343; PMCID: PMC7710830.
https://pubmed.ncbi.nlm.nih.gov/33330343/
14. de Frel DL, Atsma DE, Pijl H, Seidell JC, Leenen PJM, Dik WA, van Rossum EFC. The Impact of Obesity and Lifestyle on the Immune System and Susceptibility to Infections Such as COVID-19. Front Nutr. 2020 Nov 19;7:597600. doi: 10.3389/fnut.2020.597600. PMID: 33330597; PMCID: PMC7711810.
https://pubmed.ncbi.nlm.nih.gov/33330597/
15. Epidemiologische situatie van SARS-CoV-2 in Nederland. Rijksinstituut voor Volksgezondheid en Milieu – RIVM 2 maart 2021, 10:00. Accessed 14 april 2021.
https://www.rivm.nl/sites/default/files/2021-03/COVID-19_WebSite_rapport...
16. NICE. COVID-19 op de Nederlandse Intensive Cares; Patiëntkarakteristieken en uitkomsten vergeleken met pneumonie patiënten op de IC in 2017-2019. Accessed 14 april 2021.
https://devrijeomroep.nl/wp-content/uploads/2021/03/COVID_rapport.pdf
17. Barber C. The Problem of ‘Long Haul’ COVID. More and more patients are dealing with major symptoms that linger for months. Scientific American December 29, 2020
https://www.scientificamerican.com/article/the-problem-of-long-haul-covid/
18. Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, Pujol JC, Klaser K, Antonelli M, Canas LS, Molteni E, Modat M, Jorge Cardoso M, May A, Ganesh S, Davies R, Nguyen LH, Drew DA, Astley CM, Joshi AD, Merino J, Tsereteli N, Fall T, Gomez MF, Duncan EL, Menni C, Williams FMK, Franks PW, Chan AT, Wolf J, Ourselin S, Spector T, Steves CJ. Attributes and predictors of long COVID. Nat Med. 2021 Mar 10. doi: 10.1038/s41591-021-01292-y. Epub ahead of print. PMID: 33692530.
https://pubmed.ncbi.nlm.nih.gov/33692530/
19. Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, Cook JR, Nordvig AS, Shalev D, Sehrawat TS, Ahluwalia N, Bikdeli B, Dietz D, Der-Nigoghossian C, Liyanage-Don N, Rosner GF, Bernstein EJ, Mohan S, Beckley AA, Seres DS, Choueiri TK, Uriel N, Ausiello JC, Accili D, Freedberg DE, Baldwin M, Schwartz A, Brodie D, Garcia CK, Elkind MSV, Connors JM, Bilezikian JP, Landry DW, Wan EY. Post-acute COVID-19 syndrome. Nat Med. 2021 Mar 22. doi: 10.1038/s41591-021-01283-z. Epub ahead of print. PMID: 33753937.
https://pubmed.ncbi.nlm.nih.gov/33753937/
20. Office for National Statistics. Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK: 1 April 2021
https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/...
20a. Wong TL, Weitzer DJ. Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)-A Systemic Review and Comparison of Clinical Presentation and Symptomatology. Medicina (Kaunas). 2021 Apr 26;57(5):418. doi: 10.3390/medicina57050418. PMID: 33925784.
https://pubmed.ncbi.nlm.nih.gov/33925784/
21. Honce R, Schultz-Cherry S. Impact of Obesity on Influenza A Virus Pathogenesis, Immune Response, and Evolution. Front Immunol. 2019 May 10;10:1071. doi: 10.3389/fimmu.2019.01071. PMID: 31134099; PMCID: PMC6523028.
https://pubmed.ncbi.nlm.nih.gov/31134099/
22. Gleeson LE, Roche HM, Sheedy FJ. Obesity, COVID-19 and innate immunometabolism. Br J Nutr. 2021 Mar 28;125(6):628-632. doi: 10.1017/S0007114520003529. Epub 2020 Sep 7. PMID: 32892755; PMCID: PMC7520638.
https://pubmed.ncbi.nlm.nih.gov/32892755/
23. Badawi A, Ryoo SG. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int J Infect Dis. 2016 Aug;49:129-33. doi: 10.1016/j.ijid.2016.06.015. Epub 2016 Jun 21. PMID: 27352628; PMCID: PMC7110556.
https://pubmed.ncbi.nlm.nih.gov/27352628/
24. Pi-Sunyer X. The medical risks of obesity. Postgrad Med. 2009 Nov;121(6):21-33. doi: 10.3810/pgm.2009.11.2074. PMID: 19940414; PMCID: PMC2879283.
https://pubmed.ncbi.nlm.nih.gov/19940414/
25. Smith AG, Sheridan PA, Harp JB, Beck MA. Diet-induced obese mice have increased mortality and altered immune responses when infected with influenza virus. J Nutr. 2007 May;137(5):1236-43. doi: 10.1093/jn/137.5.1236. PMID: 17449587.
https://pubmed.ncbi.nlm.nih.gov/17449587/
26. Milner JJ, Beck MA. The impact of obesity on the immune response to infection. Proc Nutr Soc. 2012 May;71(2):298-306. doi: 10.1017/S0029665112000158. Epub 2012 Mar 14. PMID: 22414338; PMCID: PMC4791086.
https://pubmed.ncbi.nlm.nih.gov/22414338/
27. Viardot A, Heilbronn LK, Samocha-Bonet D, Mackay F, Campbell LV, Samaras K. Obesity is associated with activated and insulin resistant immune cells. Diabetes Metab Res Rev. 2012 Jul;28(5):447-54. doi: 10.1002/dmrr.2302. Epub 2012 Apr 10. PMID: 22492715.
https://pubmed.ncbi.nlm.nih.gov/22492715/
28. Green WD, Beck MA. Obesity Impairs the Adaptive Immune Response to Influenza Virus. Ann Am Thorac Soc. 2017 Nov;14(Supplement_5):S406-S409. doi: 10.1513/AnnalsATS.201706-447AW. PMID: 29161078; PMCID: PMC5711276.
https://pubmed.ncbi.nlm.nih.gov/29161078/
29. Korakas E, Ikonomidis I, Kousathana F, Balampanis K, Kountouri A, Raptis A, Palaiodimou L, Kokkinos A, Lambadiari V. Obesity and COVID-19: immune and metabolic derangement as a possible link to adverse clinical outcomes. Am J Physiol Endocrinol Metab. 2020 Jul 1;319(1):E105-E109. doi: 10.1152/ajpendo.00198.2020. Epub 2020 May 27. PMID: 32459524; PMCID: PMC7322508.
https://pubmed.ncbi.nlm.nih.gov/32459524/
30. Luzi L, Radaelli MG. Influenza and obesity: its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol. 2020 Jun;57(6):759-764. doi: 10.1007/s00592-020-01522-8. Epub 2020 Apr 5. PMID: 32249357; PMCID: PMC7130453.
https://pubmed.ncbi.nlm.nih.gov/32249357/
31. Rebello CJ, Kirwan JP, Greenway FL. Obesity, the most common comorbidity in SARS-CoV-2: is leptin the link? Int J Obes (Lond). 2020 Sep;44(9):1810-1817. doi: 10.1038/s41366-020-0640-5. Epub 2020 Jul 9. PMID: 32647360; PMCID: PMC7347260.
https://pubmed.ncbi.nlm.nih.gov/32647360/
32. Pérez-Galarza J, Prócel C, Cañadas C, Aguirre D, Pibaque R, Bedón R, Sempértegui F, Drexhage H, Baldeón L. Immune Response to SARS-CoV-2 Infection in Obesity and T2D: Literature Review. Vaccines (Basel). 2021 Jan 29;9(2):102. doi: 10.3390/vaccines9020102. PMID: 33572702; PMCID: PMC7911386.
https://pubmed.ncbi.nlm.nih.gov/33572702/
33. Brodin P. Immune determinants of COVID-19 disease presentation and severity. Nat Med. 2021 Jan;27(1):28-33. doi: 10.1038/s41591-020-01202-8. Epub 2021 Jan 13. PMID: 33442016.
https://pubmed.ncbi.nlm.nih.gov/33442016/
34. Guglielmi V, Colangeli L, D'Adamo M, Sbraccia P. Susceptibility and Severity of Viral Infections in Obesity: Lessons from Influenza to COVID-19. Does Leptin Play a Role? Int J Mol Sci. 2021 Mar 20;22(6):3183. doi: 10.3390/ijms22063183. PMID: 33804765; PMCID: PMC8003928.
https://pubmed.ncbi.nlm.nih.gov/33804765/
35. Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006 Dec 14;444(7121):860-7. doi: 10.1038/nature05485. PMID: 17167474.
https://pubmed.ncbi.nlm.nih.gov/17167474/
36. Hotamisligil GS, Erbay E. Nutrient sensing and inflammation in metabolic diseases. Nat Rev Immunol. 2008 Dec;8(12):923-34. doi: 10.1038/nri2449. PMID: 19029988; PMCID: PMC2814543.
https://pubmed.ncbi.nlm.nih.gov/19029988/
37. Calay ES, Hotamisligil GS. Turning off the inflammatory, but not the metabolic, flames. Nat Med. 2013 Mar;19(3):265-7. doi: 10.1038/nm.3114. PMID: 23467233.
https://pubmed.ncbi.nlm.nih.gov/23467233/
38. Hotamisligil GS. Inflammation, metaflammation and immunometabolic disorders. Nature. 2017 Feb 8;542(7640):177-185. doi: 10.1038/nature21363. PMID: 28179656.
https://pubmed.ncbi.nlm.nih.gov/28179656/
39. Facchini FS, Hua N, Abbasi F, Reaven GM. Insulin resistance as a predictor of age-related diseases. J Clin Endocrinol Metab. 2001 Aug;86(8):3574-8. doi: 10.1210/jcem.86.8.7763. PMID: 11502781.
https://pubmed.ncbi.nlm.nih.gov/11502781/
40. Reaven GM. The insulin resistance syndrome: definition and dietary approaches to treatment. Annu Rev Nutr. 2005;25:391-406. doi: 10.1146/annurev.nutr.24.012003.132155. PMID: 16011472.
https://pubmed.ncbi.nlm.nih.gov/16011472/
41. Reaven GM. The metabolic syndrome: requiescat in pace. Clin Chem. 2005 Jun;51(6):931-8. doi: 10.1373/clinchem.2005.048611. Epub 2005 Mar 3. PMID: 15746300.
https://pubmed.ncbi.nlm.nih.gov/15746300/
41a. Reaven G. Insulin resistance, type 2 diabetes mellitus, and cardiovascular disease: the end of the beginning. Circulation. 2005 Nov 15;112(20):3030-2. doi: 10.1161/CIRCULATIONAHA.105.504670. PMID: 16286599.
https://pubmed.ncbi.nlm.nih.gov/16286599/
41b. Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech. 2009 May-Jun;2(5-6):231-7. doi: 10.1242/dmm.001180. PMID: 19407331; PMCID: PMC2675814.
https://pubmed.ncbi.nlm.nih.gov/19407331/
42. Egger G, Dixon J. Should obesity be the main game? Or do we need an environmental makeover to combat the inflammatory and chronic disease epidemics? Obes Rev. 2009 Mar;10(2):237-49. doi: 10.1111/j.1467-789X.2008.00542.x. Epub 2008 Nov 24. PMID: 19055538.
https://pubmed.ncbi.nlm.nih.gov/19055538/
43. Egger G, Dixon J. Obesity and chronic disease: always offender or often just accomplice? Br J Nutr. 2009 Oct;102(8):1238-42. doi: 10.1017/S0007114509371676. Epub 2009 May 18. PMID: 19445817.
https://pubmed.ncbi.nlm.nih.gov/19445817/
44. Egger G, Dixon J. Inflammatory effects of nutritional stimuli: further support for the need for a big picture approach to tackling obesity and chronic disease. Obes Rev. 2010 Feb;11(2):137-49. doi: 10.1111/j.1467-789X.2009.00644.x. Epub 2009 Jul 30. PMID: 19656309.
https://pubmed.ncbi.nlm.nih.gov/19656309/
45. Egger G, Dixon J. Beyond obesity and lifestyle: a review of 21st century chronic disease determinants. Biomed Res Int. 2014;2014:731685. doi: 10.1155/2014/731685. Epub 2014 Apr 7. PMID: 24804239; PMCID: PMC3997940.
https://pubmed.ncbi.nlm.nih.gov/24804239/
46. Straub RH, Cutolo M, Buttgereit F, Pongratz G. Energy regulation and neuroendocrine-immune control in chronic inflammatory diseases. J Intern Med. 2010 Jun;267(6):543-60. doi: 10.1111/j.1365-2796.2010.02218.x. Epub 2010 Jan 28. PMID: 20210843.
https://pubmed.ncbi.nlm.nih.gov/20210843/
47. Straub RH. Concepts of evolutionary medicine and energy regulation contribute to the etiology of systemic chronic inflammatory diseases. Brain Behav Immun. 2011 Jan;25(1):1-5. doi: 10.1016/j.bbi.2010.08.002. Epub 2010 Aug 10. PMID: 20705130.
https://pubmed.ncbi.nlm.nih.gov/20705130/
48. Straub RH. Evolutionary medicine and chronic inflammatory state--known and new concepts in pathophysiology. J Mol Med (Berl). 2012 May;90(5):523-34. doi: 10.1007/s00109-012-0861-8. Epub 2012 Jan 22. PMID: 22271169; PMCID: PMC3354326.
https://pubmed.ncbi.nlm.nih.gov/22271169/
49. Straub RH, Schradin C. Chronic inflammatory systemic diseases: An evolutionary trade-off between acutely beneficial but chronically harmful programs. Evol Med Public Health. 2016 Jan 27;2016(1):37-51. doi: 10.1093/emph/eow001. PMID: 26817483; PMCID: PMC4753361.
https://pubmed.ncbi.nlm.nih.gov/26817483/
50. Straub RH. The brain and immune system prompt energy shortage in chronic inflammation and ageing. Nat Rev Rheumatol. 2017 Dec;13(12):743-751. doi: 10.1038/nrrheum.2017.172. Epub 2017 Oct 12. PMID: 29021568.
https://pubmed.ncbi.nlm.nih.gov/29021568/
51. Muskiet FAJ. De evolutionaire achtergrond, oorzaak en consequenties van chronische systemische lage graad ontsteking; betekenis voor de klinische chemie. Ned Tijdschr Klin Chem Labgeneesk 2011; 36: 199-214.
https://www.nvkc.nl/sites/default/files/NTKC/Evolutionaireachtergrondchr...
52. Muskiet FAJ, Muskiet MHA. Chronische systemische lagegraadontsteking. De opmaat voor het insulineresistentiesyndroom en sequelae. Arts Therapeut en Apotheker 2012;13(1):10-16.
https://www.voedingsgeneeskunde.nl/ata-13-1/chronische-systemische-lageg...
53. Rasmussen A. One Year In, Our Biggest Lessons and Unsolved Mysteries about COVID-19. March 11, 2021. Acessed 15 April 2021.
https://leaps.org/one-year-in-our-biggest-lessons-and-unsolved-mysteries...
54. Blanco-Melo D, Nilsson-Payant BE, Liu WC, Uhl S, Hoagland D, Møller R, Jordan TX, Oishi K, Panis M, Sachs D, Wang TT, Schwartz RE, Lim JK, Albrecht RA, tenOever BR. Imbalanced Host Response to SARS-CoV-2 Drives Development of COVID-19. Cell. 2020 May 28;181(5):1036-1045.e9. doi: 10.1016/j.cell.2020.04.026. Epub 2020 May 15. PMID: 32416070; PMCID: PMC7227586.
https://pubmed.ncbi.nlm.nih.gov/32416070/
55. Petersen E, Koopmans M, Go U, Hamer DH, Petrosillo N, Castelli F, Storgaard M, Al Khalili S, Simonsen L. Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics. Lancet Infect Dis. 2020 Sep;20(9):e238-e244. doi: 10.1016/S1473-3099(20)30484-9. Epub 2020 Jul 3. PMID: 32628905; PMCID: PMC7333991.
https://pubmed.ncbi.nlm.nih.gov/32628905/
56. RIVM. Volwassenen met overgewicht en obesitas naar leeftijd 2010 (18 jaar en ouder). Accessed 15 April 2021.
https://www.volksgezondheidenzorg.info/onderwerp/overgewicht/cijfers-con...
57. RIVM. Prevalentie diabetes in huisartsenpraktijk naar leeftijd en geslacht. Jaarprevalentie diabetes mellitus 2019. Accessed 15 April 2021.
https://www.volksgezondheidenzorg.info/onderwerp/diabetes-mellitus/cijfe...
58. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R; IDF Diabetes Atlas Committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019 Nov;157:107843. doi: 10.1016/j.diabres.2019.107843. Epub 2019 Sep 10. PMID: 31518657.
https://pubmed.ncbi.nlm.nih.gov/31518657/
59. Paolisso G, Barbieri M, Rizzo MR, Carella C, Rotondi M, Bonafè M, Franceschi C, Rose G, De Benedictis G. Low insulin resistance and preserved beta-cell function contribute to human longevity but are not associated with TH-INS genes. Exp Gerontol. 2001 Dec;37(1):149-56. doi: 10.1016/s0531-5565(01)00148-6. PMID: 11738155.
https://pubmed.ncbi.nlm.nih.gov/11738155/
60. Barbieri M, Gambardella A, Paolisso G, Varricchio M. Metabolic aspects of the extreme longevity. Exp Gerontol. 2008 Feb;43(2):74-8. doi: 10.1016/j.exger.2007.06.003. Epub 2007 Jun 30. PMID: 17697759.
https://pubmed.ncbi.nlm.nih.gov/17697759/
61. Alegría Ezquerra E, Castellano Vázquez JM, Alegría Barrero A. Obesidad, síndrome metabólico y diabetes: implicaciones cardiovasculares y actuación terapéutica [Obesity, metabolic syndrome and diabetes: cardiovascular implications and therapy]. Rev Esp Cardiol. 2008 Jul;61(7):752-64. Spanish. PMID: 18590648.
https://pubmed.ncbi.nlm.nih.gov/18590648/
62. RIVM. Prevalentie coronaire hartziekten in huisartsenpraktijk naar leeftijd en geslacht. Jaarprevalentie coronaire hartziekten 2019. Accessed 15 April 2021.
https://www.volksgezondheidenzorg.info/onderwerp/coronaire-hartziekten/c...
63. RIVM. Aantal nieuwe gevallen van kanker 2020. Accessed 15 April 2021.
https://www.volksgezondheidenzorg.info/onderwerp/kanker/cijfers-context/...
64. RIVM. Opleidingsniveau naar leeftijd 2018. Accessed 15 April 2021
https://www.volksgezondheidenzorg.info/onderwerp/sociaaleconomische-stat...
65. Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JL, Bhattoa HP. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients. 2020 Apr 2;12(4):988. doi: 10.3390/nu12040988. PMID: 32252338; PMCID: PMC7231123.
https://pubmed.ncbi.nlm.nih.gov/32252338/
66. Mercola J, Grant WB, Wagner CL. Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity. Nutrients. 2020 Oct 31;12(11):3361. doi: 10.3390/nu12113361. PMID: 33142828; PMCID: PMC7692080.
https://pubmed.ncbi.nlm.nih.gov/33142828/
67. Grant WB, Boucher BJ. Yes, vitamin D can be a magic bullet. Clin Nutr. 2020 May;39(5):1627. doi: 10.1016/j.clnu.2020.03.021. Epub 2020 Mar 31. PMID: 32280007.
https://pubmed.ncbi.nlm.nih.gov/32280007/
68. Vogel-González M, Talló-Parra M, Herrera-Fernández V, Pérez-Vilaró G, Chillón M, Nogués X, Gómez-Zorrilla S, López-Montesinos I, Arnau-Barrés I, Sorli-Redó ML, Horcajada JP, García-Giralt N, Pascual J, Díez J, Vicente R, Güerri-Fernández R. Low Zinc Levels at Admission Associates with Poor Clinical Outcomes in SARS-CoV-2 Infection. Nutrients. 2021 Feb 9;13(2):562. doi: 10.3390/nu13020562. PMID: 33572045; PMCID: PMC7914437.
https://pubmed.ncbi.nlm.nih.gov/33572045/
69. Jothimani D, Kailasam E, Danielraj S, Nallathambi B, Ramachandran H, Sekar P, Manoharan S, Ramani V, Narasimhan G, Kaliamoorthy I, Rela M. COVID-19: Poor outcomes in patients with zinc deficiency. Int J Infect Dis. 2020 Nov;100:343-349. doi: 10.1016/j.ijid.2020.09.014. Epub 2020 Sep 10. PMID: 32920234; PMCID: PMC7482607.
https://pubmed.ncbi.nlm.nih.gov/32920234/
70. Bencivenga L, Rengo G, Varricchi G. Elderly at time of COronaVIrus disease 2019 (COVID-19): possible role of immunosenescence and malnutrition. Geroscience. 2020 Aug;42(4):1089-1092. doi: 10.1007/s11357-020-00218-9. Epub 2020 Jun 23. PMID: 32578073; PMCID: PMC7308600.
https://pubmed.ncbi.nlm.nih.gov/32578073/
71. Kaufman HW, Niles JK, Kroll MH, Bi C, Holick MF. SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels. PLoS One. 2020 Sep 17;15(9):e0239252. doi: 10.1371/journal.pone.0239252. PMID: 32941512; PMCID: PMC7498100.
https://pubmed.ncbi.nlm.nih.gov/32941512/
72. Wessels I, Rolles B, Rink L. The Potential Impact of Zinc Supplementation on COVID-19 Pathogenesis. Front Immunol. 2020 Jul 10;11:1712. doi: 10.3389/fimmu.2020.01712. PMID: 32754164; PMCID: PMC7365891.
https://pubmed.ncbi.nlm.nih.gov/32754164/
73. Wessels I, Rolles B, Slusarenko AJ, Rink L. Zinc deficiency as a possible risk factor for increased susceptibility and severe progression of Corona Virus Disease 19. Br J Nutr. 2021 Mar 1:1-19. doi: 10.1017/S0007114521000738. Epub ahead of print. PMID: 33641685.
https://pubmed.ncbi.nlm.nih.gov/33641685/
74. Muthuvattur Pallath M, Ahirwar AK, Chandra Tripathi S, Asia P, Sakarde A, Gopal N. COVID-19 and nutritional deficiency: a review of existing knowledge. Horm Mol Biol Clin Investig. 2021 Feb 4;42(1):77-85. doi: 10.1515/hmbci-2020-0074. PMID: 33544528.
https://pubmed.ncbi.nlm.nih.gov/33544528/
75. Fedele D, De Francesco A, Riso S, Collo A. Obesity, malnutrition, and trace element deficiency in the coronavirus disease (COVID-19) pandemic: An overview. Nutrition. 2021 Jan;81:111016. doi: 10.1016/j.nut.2020.111016. Epub 2020 Sep 8. PMID: 33059127; PMCID: PMC7832575.
https://pubmed.ncbi.nlm.nih.gov/33059127/
76. Heller RA, Sun Q, Hackler J, Seelig J, Seibert L, Cherkezov A, Minich WB, Seemann P, Diegmann J, Pilz M, Bachmann M, Ranjbar A, Moghaddam A, Schomburg L. Prediction of survival odds in COVID-19 by zinc, age and selenoprotein P as composite biomarker. Redox Biol. 2021 Jan;38:101764. doi: 10.1016/j.redox.2020.101764. Epub 2020 Oct 20. PMID: 33126054; PMCID: PMC7574778.
https://pubmed.ncbi.nlm.nih.gov/33126054/
77. Gröber U, Holick MF. The coronavirus disease (COVID-19) - A supportive approach with selected micronutrients. Int J Vitam Nutr Res. 2021 Jan 25:1-22. doi: 10.1024/0300-9831/a000693. Epub ahead of print. PMID: 33487035.
https://pubmed.ncbi.nlm.nih.gov/33487035/
77a. Bennouar S, Cherif AB, Kessira A, Bennouar DE, Abdi S. Vitamin D Deficiency and Low Serum Calcium as Predictors of Poor Prognosis in Patients with Severe COVID-19. J Am Coll Nutr. 2021 Jan 12:1-11. doi: 10.1080/07315724.2020.1856013. Epub ahead of print. PMID: 33434117; PMCID: PMC7814570.
https://pubmed.ncbi.nlm.nih.gov/33434117/
77b. Bauer JM, Morley JE. Editorial: COVID-19 in older persons: the role of nutrition. Curr Opin Clin Nutr Metab Care. 2021 Jan;24(1):1-3. doi: 10.1097/MCO.0000000000000717. PMID: 33323712; PMCID: PMC7752213.
https://pubmed.ncbi.nlm.nih.gov/33323712/
78. Snijder MB, van Dam RM, Visser M, Deeg DJ, Dekker JM, Bouter LM, Seidell JC, Lips P. Adiposity in relation to vitamin D status and parathyroid hormone levels: a population-based study in older men and women. J Clin Endocrinol Metab. 2005 Jul;90(7):4119-23. doi: 10.1210/jc.2005-0216. Epub 2005 Apr 26. PMID: 15855256.
https://pubmed.ncbi.nlm.nih.gov/15855256/
79. Via M. The malnutrition of obesity: micronutrient deficiencies that promote diabetes. ISRN Endocrinol. 2012;2012:103472. doi: 10.5402/2012/103472. Epub 2012 Mar 15. PMID: 22462011; PMCID: PMC3313629.
https://pubmed.ncbi.nlm.nih.gov/22462011/
80. Banach W, Nitschke K, Krajewska N, Mongiałło W, Matuszak O, Muszyński J, Skrypnik D. The Association between Excess Body Mass and Disturbances in Somatic Mineral Levels. Int J Mol Sci. 2020 Oct 3;21(19):7306. doi: 10.3390/ijms21197306. PMID: 33022938; PMCID: PMC7582962.
https://pubmed.ncbi.nlm.nih.gov/33022938/
81. Astrup A, Bügel S. Overfed but undernourished: recognizing nutritional inadequacies/deficiencies in patients with overweight or obesity. Int J Obes (Lond). 2019 Feb;43(2):219-232. doi: 10.1038/s41366-018-0143-9. Epub 2018 Jul 6. PMID: 29980762.
https://pubmed.ncbi.nlm.nih.gov/29980762/
82. Dubey P, Thakur V, Chattopadhyay M. Role of Minerals and Trace Elements in Diabetes and Insulin Resistance. Nutrients. 2020 Jun 23;12(6):1864. doi: 10.3390/nu12061864. PMID: 32585827; PMCID: PMC7353202.
https://pubmed.ncbi.nlm.nih.gov/32585827/
83. Pepersack T, Rotsaert P, Benoit F, Willems D, Fuss M, Bourdoux P, Duchateau J. Prevalence of zinc deficiency and its clinical relevance among hospitalised elderly. Arch Gerontol Geriatr. 2001 Nov-Dec;33(3):243-53. doi: 10.1016/s0167-4943(01)00186-8. PMID: 15374021.
https://pubmed.ncbi.nlm.nih.gov/15374021/
84. Savarino L, Granchi D, Ciapetti G, Cenni E, Ravaglia G, Forti P, Maioli F, Mattioli R. Serum concentrations of zinc and selenium in elderly people: results in healthy nonagenarians/centenarians. Exp Gerontol. 2001 Feb;36(2):327-39. doi: 10.1016/s0531-5565(00)00218-7. PMID: 11226746.
https://pubmed.ncbi.nlm.nih.gov/11226746/
85. Sebastian RS, Cleveland LE, Goldman JD, Moshfegh AJ. Older adults who use vitamin/mineral supplements differ from nonusers in nutrient intake adequacy and dietary attitudes. J Am Diet Assoc. 2007 Aug;107(8):1322-32. doi: 10.1016/j.jada.2007.05.010. PMID: 17659898.
https://pubmed.ncbi.nlm.nih.gov/17659898/
86. Weeden A, Remig V, Holcomb CA, Herald TJ, Baybutt RC. Vitamin and mineral supplements have a nutritionally significant impact on micronutrient intakes of older adults attending senior centers. J Nutr Elder. 2010 Apr;29(2):241-54. doi: 10.1080/01639366.2010.480897. PMID: 20473815.
https://pubmed.ncbi.nlm.nih.gov/20473815/
87. Smit E, Winters-Stone KM, Loprinzi PD, Tang AM, Crespo CJ. Lower nutritional status and higher food insufficiency in frail older US adults. Br J Nutr. 2013 Jul 14;110(1):172-8. doi: 10.1017/S000711451200459X. Epub 2012 Nov 1. PMID: 23113895; PMCID: PMC4023911.
https://pubmed.ncbi.nlm.nih.gov/23113895/
88. Yasuda H, Tsutsui T. Infants and elderlies are susceptible to zinc deficiency. Sci Rep. 2016 Feb 25;6:21850. doi: 10.1038/srep21850. PMID: 26912464; PMCID: PMC4766432.
https://pubmed.ncbi.nlm.nih.gov/26912464/
89. Fantacone ML, Lowry MB, Uesugi SL, Michels AJ, Choi J, Leonard SW, Gombart SK, Gombart JS, Bobe G, Gombart AF. The Effect of a Multivitamin and Mineral Supplement on Immune Function in Healthy Older Adults: A Double-Blind, Randomized, Controlled Trial. Nutrients. 2020 Aug 14;12(8):2447. doi: 10.3390/nu12082447. PMID: 32823974; PMCID: PMC7468989.
https://pubmed.ncbi.nlm.nih.gov/32823974/
90. Rayman MP, Calder PC. Optimising COVID-19 vaccine efficacy by ensuring nutritional adequacy. Br J Nutr. 2021 Jan 28:1-2. doi: 10.1017/S0007114521000386. Epub ahead of print. PMID: 33504378; PMCID: PMC7884658.
https://pubmed.ncbi.nlm.nih.gov/33504378/
91. Calder PC, Carr AC, Gombart AF, Eggersdorfer M. Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections. Nutrients. 2020 Apr 23;12(4):1181. doi: 10.3390/nu12041181. PMID: 32340216; PMCID: PMC7230749.
https://pubmed.ncbi.nlm.nih.gov/32340216/
92. Morais AHA, Aquino JS, da Silva-Maia JK, Vale SHL, Maciel BLL, Passos TS. Nutritional status, diet and viral respiratory infections: perspectives for severe acute respiratory syndrome coronavirus 2. Br J Nutr. 2021 Apr 28;125(8):851-862. doi: 10.1017/S0007114520003311. Epub 2020 Aug 26. PMID: 32843118; PMCID: PMC7542326.
https://pubmed.ncbi.nlm.nih.gov/32843118/
93. Gombart AF, Pierre A, Maggini S. A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection. Nutrients. 2020 Jan 16;12(1):236. doi: 10.3390/nu12010236. PMID: 31963293; PMCID: PMC7019735.
https://pubmed.ncbi.nlm.nih.gov/31963293/
94. Di Renzo L, Gualtieri P, Pivari F, Soldati L, Attinà A, Leggeri C, Cinelli G, Tarsitano MG, Caparello G, Carrano E, Merra G, Pujia AM, Danieli R, De Lorenzo A. COVID-19: Is there a role for immunonutrition in obese patient? J Transl Med. 2020 Nov 7;18(1):415. doi: 10.1186/s12967-020-02594-4. PMID: 33160363; PMCID: PMC7647877.
https://pubmed.ncbi.nlm.nih.gov/33160363/
95. Tsoukalas D, Sarandi E. Micronutrient deficiencies in patients with COVID-19: how metabolomics can contribute to their prevention and replenishment. BMJ Nutr Prev Health. 2020 Nov 3;3(2):419-420. doi: 10.1136/bmjnph-2020-000169. PMID: 33521556; PMCID: PMC7841838.
https://pubmed.ncbi.nlm.nih.gov/33521556/
96. Fresán U, Guevara M, Elía F, Albéniz E, Burgui C, Castilla J; Working Group for the Study of COVID-19 in Navarra. Independent Role of Severe Obesity as a Risk Factor for COVID-19 Hospitalization: A Spanish Population-Based Cohort Study. Obesity (Silver Spring). 2021 Jan;29(1):29-37. doi: 10.1002/oby.23029. Epub 2020 Dec 6. PMID: 32885905.
https://pubmed.ncbi.nlm.nih.gov/32885905/
97. Kass DA, Duggal P, Cingolani O. Obesity could shift severe COVID-19 disease to younger ages. Lancet. 2020 May 16;395(10236):1544-1545. doi: 10.1016/S0140-6736(20)31024-2. Epub 2020 May 4. PMID: 32380044; PMCID: PMC7196905.
https://pubmed.ncbi.nlm.nih.gov/32380044/
98. Bajaj V, Gadi N, Spihlman AP, Wu SC, Choi CH, Moulton VR. Aging, Immunity, and COVID-19: How Age Influences the Host Immune Response to Coronavirus Infections? Front Physiol. 2021 Jan 12;11:571416. doi: 10.3389/fphys.2020.571416. PMID: 33510644; PMCID: PMC7835928.
https://pubmed.ncbi.nlm.nih.gov/33510644/
99. Caussy C, Pattou F, Wallet F, Simon C, Chalopin S, Telliam C, Mathieu D, Subtil F, Frobert E, Alligier M, Delaunay D, Vanhems P, Laville M, Jourdain M, Disse E; COVID Outcomes HCL Consortium and Lille COVID–Obesity Study Group. Prevalence of obesity among adult inpatients with COVID-19 in France. Lancet Diabetes Endocrinol. 2020 Jul;8(7):562-564. doi: 10.1016/S2213-8587(20)30160-1. Epub 2020 May 18. PMID: 32437642; PMCID: PMC7234780.
https://pubmed.ncbi.nlm.nih.gov/32437642/
100. Roncon L, Zuin M, Rigatelli G, Zuliani G. Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome. J Clin Virol. 2020 Jun;127:104354. doi: 10.1016/j.jcv.2020.104354. Epub 2020 Apr 9. PMID: 32305882; PMCID: PMC7195018.
https://pubmed.ncbi.nlm.nih.gov/32305882/
101. Ghoneim S, Butt MU, Hamid O, Shah A, Asaad I. The incidence of COVID-19 in patients with metabolic syndrome and non-alcoholic steatohepatitis: A population-based study. Metabol Open. 2020 Dec;8:100057. doi: 10.1016/j.metop.2020.100057. Epub 2020 Sep 9. PMID: 32924000; PMCID: PMC7480663.
https://pubmed.ncbi.nlm.nih.gov/32924000/
102. Liu Y, Yan LM, Wan L, Xiang TX, Le A, Liu JM, Peiris M, Poon LLM, Zhang W. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect Dis. 2020 Jun;20(6):656-657. doi: 10.1016/S1473-3099(20)30232-2. Epub 2020 Mar 19. PMID: 32199493; PMCID: PMC7158902.
https://pubmed.ncbi.nlm.nih.gov/32199493/
103. Honce R, Karlsson EA, Wohlgemuth N, Estrada LD, Meliopoulos VA, Yao J, Schultz-Cherry S. Obesity-Related Microenvironment Promotes Emergence of Virulent Influenza Virus Strains. mBio. 2020 Mar 3;11(2):e03341-19. doi: 10.1128/mBio.03341-19. PMID: 32127459; PMCID: PMC7064783.
https://pubmed.ncbi.nlm.nih.gov/32127459/
104. La Cava A. Leptin in inflammation and autoimmunity. Cytokine. 2017 Oct;98:51-58. doi: 10.1016/j.cyto.2016.10.011. PMID: 27916613; PMCID: PMC5453851.
https://pubmed.ncbi.nlm.nih.gov/27916613/
105. Francisco V, Pino J, Campos-Cabaleiro V, Ruiz-Fernández C, Mera A, Gonzalez-Gay MA, Gómez R, Gualillo O. Obesity, Fat Mass and Immune System: Role for Leptin. Front Physiol. 2018 Jun 1;9:640. doi: 10.3389/fphys.2018.00640. PMID: 29910742; PMCID: PMC5992476.
https://pubmed.ncbi.nlm.nih.gov/29910742/
106. Badman MK, Flier JS. The gut and energy balance: visceral allies in the obesity wars. Science. 2005 Mar 25;307(5717):1909-14. doi: 10.1126/science.1109951. PMID: 15790843.
https://pubmed.ncbi.nlm.nih.gov/15790843/
107. de Luca C, Olefsky JM. Inflammation and insulin resistance. FEBS Lett. 2008 Jan 9;582(1):97-105. doi: 10.1016/j.febslet.2007.11.057. Epub 2007 Nov 29. PMID: 18053812; PMCID: PMC2246086.
https://pubmed.ncbi.nlm.nih.gov/18053812/
108. Kolb H, Kempf K, Röhling M, Martin S. Insulin: too much of a good thing is bad. BMC Med. 2020 Aug 21;18(1):224. doi: 10.1186/s12916-020-01688-6. PMID: 32819363; PMCID: PMC7441661.
https://pubmed.ncbi.nlm.nih.gov/32819363/
109. McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007 Jul;87(3):873-904. doi: 10.1152/physrev.00041.2006. PMID: 17615391.
https://pubmed.ncbi.nlm.nih.gov/17615391/
110. Wingfield JC. Control of behavioural strategies for capricious environments. Animal Behaviour Volume 66, Issue 5, November 2003, Pages 807-816.
https://www.sciencedirect.com/science/article/abs/pii/S0003347203922986
111. McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Horm Behav. 2003 Jan;43(1):2-15. doi: 10.1016/s0018-506x(02)00024-7. PMID: 12614627.
https://pubmed.ncbi.nlm.nih.gov/12614627/
112. McEwen BS. Protection and damage from acute and chronic stress: allostasis and allostatic overload and relevance to the pathophysiology of psychiatric disorders. Ann N Y Acad Sci. 2004 Dec;1032:1-7. doi: 10.1196/annals.1314.001. PMID: 15677391.
https://pubmed.ncbi.nlm.nih.gov/15677391/
113. Huber M, Knottnerus JA, Green L, van der Horst H, Jadad AR, Kromhout D, Leonard B, Lorig K, Loureiro MI, van der Meer JW, Schnabel P, Smith R, van Weel C, Smid H. How should we define health? BMJ. 2011 Jul 26;343:d4163. doi: 10.1136/bmj.d4163. PMID: 21791490.
https://pubmed.ncbi.nlm.nih.gov/21791490/
114. Centers for Disease Control and Prevention (CDC). How COVID-19 Spreads, Updated Oct. 28, 2020, Accessed 17 April 2021
https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid...
115. Funk CD, Laferrière C, Ardakani A. A Snapshot of the Global Race for Vaccines Targeting SARS-CoV-2 and the COVID-19 Pandemic. Front Pharmacol. 2020 Jun 19;11:937. doi: 10.3389/fphar.2020.00937. PMID: 32636754; PMCID: PMC7317023.
https://pubmed.ncbi.nlm.nih.gov/32636754/
115a. Senatore V, Zarra T, Buonerba A, Choo KH, Hasan SW, Korshin G, Li CW, Ksibi M, Belgiorno V, Naddeo V. Indoor versus outdoor transmission of SARS-COV-2: environmental factors in virus spread and underestimated sources of risk. EuroMediterr J Environ Integr. 2021;6(1):30. doi: 10.1007/s41207-021-00243-w. Epub 2021 Feb 10. PMID: 33585671; PMCID: PMC7873670.
https://pubmed.ncbi.nlm.nih.gov/33585671/
116. Moriyama M, Hugentobler WJ, Iwasaki A. Seasonality of Respiratory Viral Infections. Annu Rev Virol. 2020 Sep 29;7(1):83-101. doi: 10.1146/annurev-virology-012420-022445. Epub 2020 Mar 20. PMID: 32196426.
https://pubmed.ncbi.nlm.nih.gov/32196426/
116a. Morawska L, Allen J, Bahnfleth W, Bluyssen PM, Boerstra A, Buonanno G, Cao J, Dancer SJ, Floto A, Franchimon F, Greenhalgh T, Haworth C, Hogeling J, Isaxon C, Jimenez JL, Kurnitski J, Li Y, Loomans M, Marks G, Marr LC, Mazzarella L, Melikov AK, Miller S, Milton DK, Nazaroff W, Nielsen PV, Noakes C, Peccia J, Prather K, Querol X, Sekhar C, Seppänen O, Tanabe SI, Tang JW, Tellier R, Tham KW, Wargocki P, Wierzbicka A, Yao M. A paradigm shift to combat indoor respiratory infection. Science. 2021 May 14;372(6543):689-691. doi: 10.1126/science.abg2025. PMID: 33986171.
https://pubmed.ncbi.nlm.nih.gov/33986171/
117. Courtney JM, Bax A. Hydrating the respiratory tract: An alternative explanation why masks lower severity of COVID-19. Biophys J. 2021 Mar 16;120(6):994-1000. doi: 10.1016/j.bpj.2021.02.002. Epub 2021 Feb 12. PMID: 33582134; PMCID: PMC7879047.
https://pubmed.ncbi.nlm.nih.gov/33582134/
118. Wang C, Wang Z, Wang G, Lau JY, Zhang K, Li W. COVID-19 in early 2021: current status and looking forward. Signal Transduct Target Ther. 2021 Mar 8;6(1):114. doi: 10.1038/s41392-021-00527-1. PMID: 33686059; PMCID: PMC7938042.
https://pubmed.ncbi.nlm.nih.gov/33686059/
119. Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020 Apr 16;181(2):271-280.e8. doi: 10.1016/j.cell.2020.02.052. Epub 2020 Mar 5. PMID: 32142651; PMCID: PMC7102627.
https://pubmed.ncbi.nlm.nih.gov/32142651/
120. Ni W, Yang X, Yang D, Bao J, Li R, Xiao Y, Hou C, Wang H, Liu J, Yang D, Xu Y, Cao Z, Gao Z. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit Care. 2020 Jul 13;24(1):422. doi: 10.1186/s13054-020-03120-0. PMID: 32660650; PMCID: PMC7356137.
https://pubmed.ncbi.nlm.nih.gov/32660650/
121. Clausen TM, Sandoval DR, Spliid CB, Pihl J, Perrett HR, Painter CD, Narayanan A, Majowicz SA, Kwong EM, McVicar RN, Thacker BE, Glass CA, Yang Z, Torres JL, Golden GJ, Bartels PL, Porell RN, Garretson AF, Laubach L, Feldman J, Yin X, Pu Y, Hauser BM, Caradonna TM, Kellman BP, Martino C, Gordts PLSM, Chanda SK, Schmidt AG, Godula K, Leibel SL, Jose J, Corbett KD, Ward AB, Carlin AF, Esko JD. SARS-CoV-2 Infection Depends on Cellular Heparan Sulfate and ACE2. Cell. 2020 Nov 12;183(4):1043-1057.e15. doi: 10.1016/j.cell.2020.09.033. Epub 2020 Sep 14. PMID: 32970989; PMCID: PMC7489987.
https://pubmed.ncbi.nlm.nih.gov/32970989/
122. Scialo F, Daniele A, Amato F, Pastore L, Matera MG, Cazzola M, Castaldo G, Bianco A. ACE2: The Major Cell Entry Receptor for SARS-CoV-2. Lung. 2020 Dec;198(6):867-877. doi: 10.1007/s00408-020-00408-4. Epub 2020 Nov 10. PMID: 33170317; PMCID: PMC7653219.
https://pubmed.ncbi.nlm.nih.gov/33170317/
123. Medina-Enríquez MM, Lopez-León S, Carlos-Escalante JA, Aponte-Torres Z, Cuapio A, Wegman-Ostrosky T. ACE2: the molecular doorway to SARS-CoV-2. Cell Biosci. 2020 Dec 30;10(1):148. doi: 10.1186/s13578-020-00519-8. PMID: 33380340; PMCID: PMC7772801.
https://pubmed.ncbi.nlm.nih.gov/33380340/
123a. Foresta C, Rocca MS, Di Nisio A. Gender susceptibility to COVID-19: a review of the putative role of sex hormones and X chromosome. J Endocrinol Invest. 2021 May;44(5):951-956. doi: 10.1007/s40618-020-01383-6. Epub 2020 Sep 16. PMID: 32936429; PMCID: PMC7492232.
https://pubmed.ncbi.nlm.nih.gov/32936429/
124. Gupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Sehrawat TS, Bikdeli B, Ahluwalia N, Ausiello JC, Wan EY, Freedberg DE, Kirtane AJ, Parikh SA, Maurer MS, Nordvig AS, Accili D, Bathon JM, Mohan S, Bauer KA, Leon MB, Krumholz HM, Uriel N, Mehra MR, Elkind MSV, Stone GW, Schwartz A, Ho DD, Bilezikian JP, Landry DW. Extrapulmonary manifestations of COVID-19. Nat Med. 2020 Jul;26(7):1017-1032. doi: 10.1038/s41591-020-0968-3. Epub 2020 Jul 10. PMID: 32651579.
https://pubmed.ncbi.nlm.nih.gov/32651579/
125. Muus et al. Single-cell meta-analysis of SARS-CoV-2 entry genes across tissues and demographics. Nat Med. 2021 Mar;27(3):546-559. doi: 10.1038/s41591-020-01227-z. Epub 2021 Mar 2. PMID: 33654293.
https://pubmed.ncbi.nlm.nih.gov/33654293/
126. Glowacka I, Bertram S, Müller MA, Allen P, Soilleux E, Pfefferle S, Steffen I, Tsegaye TS, He Y, Gnirss K, Niemeyer D, Schneider H, Drosten C, Pöhlmann S. Evidence that TMPRSS2 activates the severe acute respiratory syndrome coronavirus spike protein for membrane fusion and reduces viral control by the humoral immune response. J Virol. 2011 May;85(9):4122-34. doi: 10.1128/JVI.02232-10. Epub 2011 Feb 16. PMID: 21325420; PMCID: PMC3126222.
https://pubmed.ncbi.nlm.nih.gov/21325420/
126a. Senapati S, Banerjee P, Bhagavatula S, Kushwaha PP, Kumar S. Contributions of human ACE2 and TMPRSS2 in determining host-pathogen interaction of COVID-19. J Genet. 2021;100(1):12. doi: 10.1007/s12041-021-01262-w. PMID: 33707363; PMCID: PMC7904510.
https://pubmed.ncbi.nlm.nih.gov/33707363/
127. Cantuti-Castelvetri L, Ojha R, Pedro LD, Djannatian M, Franz J, Kuivanen S, van der Meer F, Kallio K, Kaya T, Anastasina M, Smura T, Levanov L, Szirovicza L, Tobi A, Kallio-Kokko H, Österlund P, Joensuu M, Meunier FA, Butcher SJ, Winkler MS, Mollenhauer B, Helenius A, Gokce O, Teesalu T, Hepojoki J, Vapalahti O, Stadelmann C, Balistreri G, Simons M. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science. 2020 Nov 13;370(6518):856-860. doi: 10.1126/science.abd2985. Epub 2020 Oct 20. PMID: 33082293; PMCID: PMC7857391.
https://pubmed.ncbi.nlm.nih.gov/33082293/
128. Wetenschap onthult hoe het coronavirus onze cellen kraakt. Het virus blijkt in zekere zin niet één, maar twee huissleutels te hebben. Accessed 17 April 2021.
https://www.scientias.nl/wetenschap-onthult-hoe-het-coronavirus-onze-cel...
129. Mayi BS, Leibowitz JA, Woods AT, Ammon KA, Liu AE, Raja A. The role of Neuropilin-1 in COVID-19. PLoS Pathog. 2021 Jan 4;17(1):e1009153. doi: 10.1371/journal.ppat.1009153. PMID: 33395426; PMCID: PMC7781380.
https://pubmed.ncbi.nlm.nih.gov/33395426/
130. Libby P, Lüscher T. COVID-19 is, in the end, an endothelial disease. Eur Heart J. 2020 Sep 1;41(32):3038-3044. doi: 10.1093/eurheartj/ehaa623. PMID: 32882706; PMCID: PMC7470753.
https://pubmed.ncbi.nlm.nih.gov/32882706/
131. Pinto BGG, Oliveira AER, Singh Y, Jimenez L, Gonçalves ANA, Ogava RLT, Creighton R, Schatzmann Peron JP, Nakaya HI. ACE2 Expression Is Increased in the Lungs of Patients With Comorbidities Associated With Severe COVID-19. J Infect Dis. 2020 Jul 23;222(4):556-563. doi: 10.1093/infdis/jiaa332. PMID: 32526012; PMCID: PMC7377288.
https://pubmed.ncbi.nlm.nih.gov/32526012/
132. Volz E, Hill V, McCrone JT, Price A, Jorgensen D, O'Toole Á, Southgate J, Johnson R, Jackson B, Nascimento FF, Rey SM, Nicholls SM, Colquhoun RM, da Silva Filipe A, Shepherd J, Pascall DJ, Shah R, Jesudason N, Li K, Jarrett R, Pacchiarini N, Bull M, Geidelberg L, Siveroni I; COG-UK Consortium, Goodfellow I, Loman NJ, Pybus OG, Robertson DL, Thomson EC, Rambaut A, Connor TR. Evaluating the Effects of SARS-CoV-2 Spike Mutation D614G on Transmissibility and Pathogenicity. Cell. 2021 Jan 7;184(1):64-75.e11. doi: 10.1016/j.cell.2020.11.020. Epub 2020 Nov 19. PMID: 33275900; PMCID: PMC7674007.
https://pubmed.ncbi.nlm.nih.gov/33275900/
133. Challen R, Brooks-Pollock E, Read JM, Dyson L, Tsaneva-Atanasova K, Danon L. Risk of mortality in patients infected with SARS-CoV-2 variant of concern 202012/1: matched cohort study. BMJ. 2021 Mar 9;372:n579. doi: 10.1136/bmj.n579. PMID: 33687922; PMCID: PMC7941603.
https://pubmed.ncbi.nlm.nih.gov/33687922/
134. Graham MS, Sudre CH, May A, Antonelli M, Murray B, Varsavsky T, Kläser K, Canas LS, Molteni E, Modat M, Drew DA, Nguyen LH, Polidori L, Selvachandran S, Hu C, Capdevila J; COVID-19 Genomics UK (COG-UK) Consortium, Hammers A, Chan AT, Wolf J, Spector TD, Steves CJ, Ourselin S. Changes in symptomatology, reinfection, and transmissibility associated with the SARS-CoV-2 variant B.1.1.7: an ecological study. Lancet Public Health. 2021 Apr 12:S2468-2667(21)00055-4. doi: 10.1016/S2468-2667(21)00055-4. Epub ahead of print. PMID: 33857453; PMCID: PMC8041365.
https://pubmed.ncbi.nlm.nih.gov/33857453/
135. Frampton D, Rampling T, Cross A, Bailey H, Heaney J, Byott M, Scott R, Sconza R, Price J, Margaritis M, Bergstrom M, Spyer MJ, Miralhes PB, Grant P, Kirk S, Valerio C, Mangera Z, Prabhahar T, Moreno-Cuesta J, Arulkumaran N, Singer M, Shin GY, Sanchez E, Paraskevopoulou SM, Pillay D, McKendry RA, Mirfenderesky M, Houlihan CF, Nastouli E. Genomic characteristics and clinical effect of the emergent SARS-CoV-2 B.1.1.7 lineage in London, UK: a whole-genome sequencing and hospital-based cohort study. Lancet Infect Dis. 2021 Apr 12:S1473-3099(21)00170-5. doi: 10.1016/S1473-3099(21)00170-5. Epub ahead of print. PMID: 33857406; PMCID: PMC8041359.
https://pubmed.ncbi.nlm.nih.gov/33857406/
136. COVID-19: 'No Evidence' That UK Variant Causes More Severe Disease. Medscape, 13 April 2021. Accessed 17 April 2021.
https://www.medscape.com/viewarticle/949163
137. Melenotte C, Silvin A, Goubet AG, Lahmar I, Dubuisson A, Zumla A, Raoult D, Merad M, Gachot B, Hénon C, Solary E, Fontenay M, André F, Maeurer M, Ippolito G, Piacentini M, Wang FS, Ginhoux F, Marabelle A, Kroemer G, Derosa L, Zitvogel L. Immune responses during COVID-19 infection. Oncoimmunology. 2020 Aug 25;9(1):1807836. doi: 10.1080/2162402X.2020.1807836. PMID: 32939324; PMCID: PMC7480812.
https://pubmed.ncbi.nlm.nih.gov/32939324/
137a. Loganathan S, Kuppusamy M, Wankhar W, Gurugubelli KR, Mahadevappa VH, Lepcha L, Choudhary AK. Angiotensin-converting enzyme 2 (ACE2): COVID 19 gate way to multiple organ failure syndromes. Respir Physiol Neurobiol. 2021 Jan;283:103548. doi: 10.1016/j.resp.2020.103548. Epub 2020 Sep 18. PMID: 32956843; PMCID: PMC7500408.
https://pubmed.ncbi.nlm.nih.gov/32956843/
138. Abbasi J. Researchers Investigate What COVID-19 Does to the Heart. JAMA. 2021 Mar 2;325(9):808-811. doi: 10.1001/jama.2021.0107. PMID: 33566089.
https://pubmed.ncbi.nlm.nih.gov/33566089/
139. Davies J, Randeva HS, Chatha K, Hall M, Spandidos DA, Karteris E, Kyrou I. Neuropilin‑1 as a new potential SARS‑CoV‑2 infection mediator implicated in the neurologic features and central nervous system involvement of COVID‑19. Mol Med Rep. 2020 Nov;22(5):4221-4226. doi: 10.3892/mmr.2020.11510. Epub 2020 Sep 15. PMID: 33000221; PMCID: PMC7533503.
https://pubmed.ncbi.nlm.nih.gov/33000221/
140. Finsterer J, Scorza FA. Clinical and Pathophysiologic Spectrum of Neuro-COVID. Mol Neurobiol. 2021 Apr 8:1–5. doi: 10.1007/s12035-021-02383-0. Epub ahead of print. PMID: 33829393; PMCID: PMC8026389.
https://pubmed.ncbi.nlm.nih.gov/33829393/
141. Lima M, Siokas V, Aloizou AM, Liampas I, Mentis AA, Tsouris Z, Papadimitriou A, Mitsias PD, Tsatsakis A, Bogdanos DP, Baloyannis SJ, Dardiotis E. Unraveling the Possible Routes of SARS-COV-2 Invasion into the Central Nervous System. Curr Treat Options Neurol. 2020;22(11):37. doi: 10.1007/s11940-020-00647-z. Epub 2020 Sep 25. PMID: 32994698; PMCID: PMC7515807.
https://pubmed.ncbi.nlm.nih.gov/32994698/
142. Song X, Hu W, Yu H, Zhao L, Zhao Y, Zhao X, Xue HH, Zhao Y. Little to no expression of angiotensin-converting enzyme-2 on most human peripheral blood immune cells but highly expressed on tissue macrophages. Cytometry A. 2020 Dec 6. doi: 10.1002/cyto.a.24285. Epub ahead of print. PMID: 33280254.
https://pubmed.ncbi.nlm.nih.gov/33280254/
143. Abassi Z, Knaney Y, Karram T, Heyman SN. The Lung Macrophage in SARS-CoV-2 Infection: A Friend or a Foe? Front Immunol. 2020 Jun 5;11:1312. doi: 10.3389/fimmu.2020.01312. PMID: 32582222; PMCID: PMC7291598.
https://pubmed.ncbi.nlm.nih.gov/32582222/
144. Ryan PM, Caplice NM. Is Adipose Tissue a Reservoir for Viral Spread, Immune Activation, and Cytokine Amplification in Coronavirus Disease 2019? Obesity (Silver Spring). 2020 Jul;28(7):1191-1194. doi: 10.1002/oby.22843. Epub 2020 May 31. PMID: 32314868; PMCID: PMC7264526.
https://pubmed.ncbi.nlm.nih.gov/32314868/
145. Solomon T. Neurological infection with SARS-CoV-2 - the story so far. Nat Rev Neurol. 2021 Feb;17(2):65-66. doi: 10.1038/s41582-020-00453-w. PMID: 33414554; PMCID: PMC7789883.
https://pubmed.ncbi.nlm.nih.gov/33414554/
146. Hoagland DA, Møller R, Uhl SA, Oishi K, Frere J, Golynker I, Horiuchi S, Panis M, Blanco-Melo D, Sachs D, Arkun K, Lim JK, tenOever BR. Leveraging the antiviral type I interferon system as a first line of defense against SARS-CoV-2 pathogenicity. Immunity. 2021 Mar 9;54(3):557-570.e5. doi: 10.1016/j.immuni.2021.01.017. Epub 2021 Jan 29. PMID: 33577760; PMCID: PMC7846242.
https://pubmed.ncbi.nlm.nih.gov/33577760/
147. Samavati L, Uhal BD. ACE2, Much More Than Just a Receptor for SARS-COV-2. Front Cell Infect Microbiol. 2020 Jun 5;10:317. doi: 10.3389/fcimb.2020.00317. PMID: 32582574; PMCID: PMC7294848.
https://pubmed.ncbi.nlm.nih.gov/32582574/
148. Yanai H. Metabolic Syndrome and COVID-19. Cardiol Res. 2020 Dec;11(6):360-365. doi: 10.14740/cr1181. Epub 2020 Nov 2. PMID: 33224380; PMCID: PMC7666594.
https://pubmed.ncbi.nlm.nih.gov/33224380/
149. Bourgonje AR, Abdulle AE, Timens W, Hillebrands JL, Navis GJ, Gordijn SJ, Bolling MC, Dijkstra G, Voors AA, Osterhaus AD, van der Voort PH, Mulder DJ, van Goor H. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). J Pathol. 2020 Jul;251(3):228-248. doi: 10.1002/path.5471. Epub 2020 Jun 10. PMID: 32418199; PMCID: PMC7276767.
https://pubmed.ncbi.nlm.nih.gov/32418199/
150. Dasgupta A. Is a Bradykinin Storm Brewing in COVID-19? The scientist 26 August 2020. Accessed 17 April 2021.
https://www.the-scientist.com/news-opinion/is-a-bradykinin-storm-brewing...
151. Cevik M, Tate M, Lloyd O, Maraolo AE, Schafers J, Ho A. SARS-CoV-2, SARS-CoV, and MERS-CoV viral load dynamics, duration of viral shedding, and infectiousness: a systematic review and meta-analysis. Lancet Microbe. 2021 Jan;2(1):e13-e22. doi: 10.1016/S2666-5247(20)30172-5. Epub 2020 Nov 19. PMID: 33521734; PMCID: PMC7837230.
https://pubmed.ncbi.nlm.nih.gov/33521734/
152. Matricardi PM, Dal Negro RW, Nisini R. The first, holistic immunological model of COVID-19: Implications for prevention, diagnosis, and public health measures. Pediatr Allergy Immunol. 2020 Jul;31(5):454-470. doi: 10.1111/pai.13271. Epub 2020 Jun 5. PMID: 32359201; PMCID: PMC7267459.
https://pubmed.ncbi.nlm.nih.gov/32359201/
153. Ke R, Romero-Severson E, Sanche S, Hengartner N. Estimating the reproductive number R0 of SARS-CoV-2 in the United States and eight European countries and implications for vaccination. J Theor Biol. 2021 May 21;517:110621. doi: 10.1016/j.jtbi.2021.110621. Epub 2021 Feb 13. PMID: 33587929; PMCID: PMC7880839.
https://pubmed.ncbi.nlm.nih.gov/33587929/
154. Van Egeren D, Novokhodko A, Stoddard M, Tran U, Zetter B, Rogers M, Pentelute BL, Carlson JM, Hixon M, Joseph-McCarthy D, Chakravarty A. Risk of evolutionary escape from neutralizing antibodies targeting SARS-CoV-2 spike protein..MedRxiv preprint doi: https://doi.org/10.1101/2020.11.17.20233726; this version posted December 11, 2020
https://www.medrxiv.org/content/10.1101/2020.11.17.20233726v2
155. Cooper V. The Coronavirus Variants Don’t Seem to Be Highly Variable So Far. SARS-CoV-2 may be settling into a limited set of mutations. Scientific American, March 24, 2021.
https://www.scientificamerican.com/article/the-coronavirus-variants-dont...
156. Johansson MA, Quandelacy TM, Kada S, Prasad PV, Steele M, Brooks JT, Slayton RB, Biggerstaff M, Butler JC. SARS-CoV-2 Transmission From People Without COVID-19 Symptoms. JAMA Netw Open. 2021 Jan 4;4(1):e2035057. doi: 10.1001/jamanetworkopen.2020.35057. Erratum in: JAMA Netw Open. 2021 Feb 1;4(2):e211383. PMID: 33410879; PMCID: PMC7791354.
https://pubmed.ncbi.nlm.nih.gov/33410879/
157. Denning DW, Kilcoyne A, Ucer C. Non-infectious status indicated by detectable IgG antibody to SARS-CoV-2. Br Dent J. 2020 Oct;229(8):521-524. doi: 10.1038/s41415-020-2228-9. Epub 2020 Oct 23. PMID: 33097885; PMCID: PMC7582419.
https://pubmed.ncbi.nlm.nih.gov/33097885/
158. Lau EHY, Tsang OTY, Hui DSC, Kwan MYW, Chan WH, Chiu SS, Ko RLW, Chan KH, Cheng SMS, Perera RAPM, Cowling BJ, Poon LLM, Peiris M. Neutralizing antibody titres in SARS-CoV-2 infections. Nat Commun. 2021 Jan 4;12(1):63. doi: 10.1038/s41467-020-20247-4. PMID: 33397909; PMCID: PMC7782739.
https://pubmed.ncbi.nlm.nih.gov/33397909/
158a. Lucas C, Klein J, Sundaram M, Liu F, Wong P, Silva J, Mao T, Oh JE, Tokuyama M, Lu P, Venkataraman A, Park A, Israelow B, Wyllie AL, Vogels CBF, Muenker MC, Casanovas-Massana A, Schulz WL, Zell J, Campbell M, Fournier JB, Grubaugh ND, Farhadian S, Wisnewski AV, Cruz CD, Omer S, Ko AI, Ring A, Iwasaki A. Kinetics of antibody responses dictate COVID-19 outcome. medRxiv [Preprint]. 2020 Dec 22:2020.12.18.20248331. doi: 10.1101/2020.12.18.20248331. PMID: 33398304; PMCID: PMC7781347.
https://pubmed.ncbi.nlm.nih.gov/33398304/
158b. Larsen MD, de Graaf EL, Sonneveld ME, Plomp HR, Nouta J, Hoepel W, Chen HJ, Linty F, Visser R, Brinkhaus M, Šuštić T, de Taeye SW, Bentlage AEH, Toivonen S, Koeleman CAM, Sainio S, Kootstra NA, Brouwer PJM, Geyer CE, Derksen NIL, Wolbink G, de Winther M, Sanders RW, van Gils MJ, de Bruin S, Vlaar APJ; Amsterdam UMC COVID-19; biobank study group, Rispens T, den Dunnen J, Zaaijer HL, Wuhrer M, Ellen van der Schoot C, Vidarsson G. Afucosylated IgG characterizes enveloped viral responses and correlates with COVID-19 severity. Science. 2021 Feb 26;371(6532):eabc8378. doi: 10.1126/science.abc8378. Epub 2020 Dec 23. PMID: 33361116; PMCID: PMC7919849.
https://pubmed.ncbi.nlm.nih.gov/33361116/
158c. Štambuk T, Klasić M, Zoldoš V, Lauc G. N-glycans as functional effectors of genetic and epigenetic disease risk. Mol Aspects Med. 2020 Aug 26:100891. doi: 10.1016/j.mam.2020.100891. Epub ahead of print. PMID: 32861467.
https://pubmed.ncbi.nlm.nih.gov/32861467/
159. Marik P. COVID-19 management protocol. An overview of the MATH+ and I-MASK+ protocols. December 27, 2020.
https://www.evms.edu/media/evms_public/departments/internal_medicine/Mar...
160. Marik PE, Kory P, Varon J, Iglesias J, Meduri GU. MATH+ protocol for the treatment of SARS-CoV-2 infection: the scientific rationale. Expert Rev Anti Infect Ther. 2021 Feb;19(2):129-135. doi: 10.1080/14787210.2020.1808462. Epub 2020 Aug 18. PMID: 32809870.
https://pubmed.ncbi.nlm.nih.gov/32809870/
161. Kory P, Meduri GU, Iglesias J, Varon J, Marik PE. Clinical and Scientific Rationale for the "MATH+" Hospital Treatment Protocol for COVID-19. J Intensive Care Med. 2021 Feb;36(2):135-156. doi: 10.1177/0885066620973585. Epub 2020 Dec 15. PMID: 33317385.
https://pubmed.ncbi.nlm.nih.gov/33317385/
162. Tisoncik JR, Korth MJ, Simmons CP, Farrar J, Martin TR, Katze MG. Into the eye of the cytokine storm. Microbiol Mol Biol Rev. 2012 Mar;76(1):16-32. doi: 10.1128/MMBR.05015-11. PMID: 22390970; PMCID: PMC3294426.
https://pubmed.ncbi.nlm.nih.gov/22390970/
163. Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ; HLH Across Speciality Collaboration, UK. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020 Mar 28;395(10229):1033-1034. doi: 10.1016/S0140-6736(20)30628-0. Epub 2020 Mar 16. PMID: 32192578; PMCID: PMC7270045.
https://pubmed.ncbi.nlm.nih.gov/32192578/
164. Meftahi GH, Jangravi Z, Sahraei H, Bahari Z. The possible pathophysiology mechanism of cytokine storm in elderly adults with COVID-19 infection: the contribution of "inflame-aging". Inflamm Res. 2020 Sep;69(9):825-839. doi: 10.1007/s00011-020-01372-8. Epub 2020 Jun 11. PMID: 32529477; PMCID: PMC7289226.
https://pubmed.ncbi.nlm.nih.gov/32529477/
165. Panigrahy D, Gilligan MM, Huang S, Gartung A, Cortés-Puch I, Sime PJ, Phipps RP, Serhan CN, Hammock BD. Inflammation resolution: a dual-pronged approach to averting cytokine storms in COVID-19? Cancer Metastasis Rev. 2020 Jun;39(2):337-340. doi: 10.1007/s10555-020-09889-4. PMID: 32385712; PMCID: PMC7207990.
https://pubmed.ncbi.nlm.nih.gov/32385712/
166. Dance A. What is a cytokine storm? 19 April 2020. Accessed 18 April 2021
https://www.asbmb.org/asbmb-today/science/041920/what-is-a-cytokine-storm
167. Fajgenbaum DC, June CH. Cytokine Storm. N Engl J Med. 2020 Dec 3;383(23):2255-2273. doi: 10.1056/NEJMra2026131. PMID: 33264547; PMCID: PMC7727315.
https://pubmed.ncbi.nlm.nih.gov/33264547/
168. Bhaskar S, Sinha A, Banach M, Mittoo S, Weissert R, Kass JS, Rajagopal S, Pai AR, Kutty S. Cytokine Storm in COVID-19-Immunopathological Mechanisms, Clinical Considerations, and Therapeutic Approaches: The REPROGRAM Consortium Position Paper. Front Immunol. 2020 Jul 10;11:1648. doi: 10.3389/fimmu.2020.01648. PMID: 32754159; PMCID: PMC7365905.
https://pubmed.ncbi.nlm.nih.gov/32754159/
169. Ye Q, Wang B, Mao J. The pathogenesis and treatment of the `Cytokine Storm' in COVID-19. J Infect. 2020 Jun;80(6):607-613. doi: 10.1016/j.jinf.2020.03.037. Epub 2020 Apr 10. PMID: 32283152; PMCID: PMC7194613.
https://pubmed.ncbi.nlm.nih.gov/32283152/
170. Larenas-Linnemann D, Rodríguez-Pérez N, Arias-Cruz A, Blandón-Vijil MV, Del Río-Navarro BE, Estrada-Cardona A, Gereda JE, Luna-Pech JA, Navarrete-Rodríguez EM, Onuma-Takane E, Pozo-Beltrán CF, Rojo-Gutiérrez MI. Enhancing innate immunity against virus in times of COVID-19: Trying to untangle facts from fictions. World Allergy Organ J. 2020 Nov;13(11):100476. doi: 10.1016/j.waojou.2020.100476. Epub 2020 Oct 9. PMID: 33072240; PMCID: PMC7546230.
https://pubmed.ncbi.nlm.nih.gov/33072240/
171. Netea MG, Giamarellos-Bourboulis EJ, Domínguez-Andrés J, Curtis N, van Crevel R, van de Veerdonk FL, Bonten M. Trained Immunity: a Tool for Reducing Susceptibility to and the Severity of SARS-CoV-2 Infection. Cell. 2020 May 28;181(5):969-977. doi: 10.1016/j.cell.2020.04.042. Epub 2020 May 4. PMID: 32437659; PMCID: PMC7196902.
https://pubmed.ncbi.nlm.nih.gov/32437659/
172. Ombrello MJ, Schulert GS. COVID-19 and cytokine storm syndrome: are there lessons from macrophage activation syndrome? Transl Res. 2021 Mar 5:S1931-5244(21)00052-9. doi: 10.1016/j.trsl.2021.03.002. Epub ahead of print. PMID: 33684592; PMCID: PMC7934701
https://pubmed.ncbi.nlm.nih.gov/33684592/
173. Levi M, van der Poll T. Inflammation and coagulation. Crit Care Med. 2010 Feb;38(2 Suppl):S26-34. doi: 10.1097/CCM.0b013e3181c98d21. PMID: 20083910.
https://pubmed.ncbi.nlm.nih.gov/20083910/
174. Savla SR, Prabhavalkar KS, Bhatt LK. Cytokine storm associated coagulation complications in COVID-19 patients: Pathogenesis and Management. Expert Rev Anti Infect Ther. 2021 Apr 9. doi: 10.1080/14787210.2021.1915129. Epub ahead of print. PMID: 33832398.
https://pubmed.ncbi.nlm.nih.gov/33832398/
175. Johnson RM, Vinetz JM. Dexamethasone in the management of covid -19. BMJ. 2020 Jul 3;370:m2648. doi: 10.1136/bmj.m2648. PMID: 32620554.
https://pubmed.ncbi.nlm.nih.gov/32620554/
176. Langford BJ, So M, Raybardhan S, Leung V, Westwood D, MacFadden DR, Soucy JR, Daneman N. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020 Dec;26(12):1622-1629. doi: 10.1016/j.cmi.2020.07.016. Epub 2020 Jul 22. PMID: 32711058; PMCID: PMC7832079.
https://pubmed.ncbi.nlm.nih.gov/32711058/
177. Lansbury L, Lim B, Baskaran V, Lim WS. Co-infections in people with COVID-19: a systematic review and meta-analysis. J Infect. 2020 Aug;81(2):266-275. doi: 10.1016/j.jinf.2020.05.046. Epub 2020 May 27. PMID: 32473235; PMCID: PMC7255350.
https://pubmed.ncbi.nlm.nih.gov/32473235/
178. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Feb 15;395(10223):497-506. doi: 10.1016/S0140-6736(20)30183-5. Epub 2020 Jan 24. Erratum in: Lancet. 2020 Jan 30;: PMID: 31986264; PMCID: PMC7159299.
https://pubmed.ncbi.nlm.nih.gov/31986264/
179. Iwasaki A, Wong P. The Immune Havoc of COVID-19. The virus flourishes by undermining the body’s chemical defense system. January 1, 2021. Accessed 18 April 2021.
https://www.scientificamerican.com/article/the-immune-havoc-of-covid-19/
180. Carvalho T, Krammer F, Iwasaki A. The first 12 months of COVID-19: a timeline of immunological insights. Nat Rev Immunol. 2021 Apr;21(4):245-256. doi: 10.1038/s41577-021-00522-1. Epub 2021 Mar 15. PMID: 33723416; PMCID: PMC7958099.
https://pubmed.ncbi.nlm.nih.gov/33723416/
181. Jarjour NN, Masopust D, Jameson SC. T Cell Memory: Understanding COVID-19. Immunity. 2021 Jan 12;54(1):14-18. doi: 10.1016/j.immuni.2020.12.009. Epub 2020 Dec 19. PMID: 33406391; PMCID: PMC7749639.
https://pubmed.ncbi.nlm.nih.gov/33406391/
182. Cavaillon, J.‐M. (2015). Molecular Mediators: Cytokines. In Reviews in Cell Biology and Molecular Medicine, R.A. Meyers (Ed.).
https://doi.org/10.1002/3527600906.mcb.200400134.pub2
183. Dan JM, Mateus J, Kato Y, Hastie KM, Yu ED, Faliti CE, Grifoni A, Ramirez SI, Haupt S, Frazier A, Nakao C, Rayaprolu V, Rawlings SA, Peters B, Krammer F, Simon V, Saphire EO, Smith DM, Weiskopf D, Sette A, Crotty S. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science. 2021 Feb 5;371(6529):eabf4063. doi: 10.1126/science.abf4063. Epub 2021 Jan 6. PMID: 33408181; PMCID: PMC7919858.
https://pubmed.ncbi.nlm.nih.gov/33408181/
184. Plüddemann A, Aronson JK. COVID-19 infection? Why immunity is about more than antibodies October 19, 2020. Accessed 18 April 2021
https://www.cebm.net/covid-19/what-is-the-role-of-t-cells-in-covid-19-in...
185. Ieronymaki E, Daskalaki MG, Lyroni K, Tsatsanis C. Insulin Signaling and Insulin Resistance Facilitate Trained Immunity in Macrophages Through Metabolic and Epigenetic Changes. Front Immunol. 2019 Jun 12;10:1330. doi: 10.3389/fimmu.2019.01330. PMID: 31244863; PMCID: PMC6581697.
https://pubmed.ncbi.nlm.nih.gov/31244863/
186. Moorlag SJCFM, van Deuren RC, van Werkhoven CH, Jaeger M, Debisarun P, Taks E, Mourits VP, Koeken VACM, de Bree LCJ, Ten Doesschate T, Cleophas MC, Smeekens S, Oosting M, van de Veerdonk FL, Joosten LAB, Ten Oever J, van der Meer JWM, Curtis N, Aaby P, Stabell-Benn C, Giamarellos-Bourboulis EJ, Bonten M, van Crevel R, Netea MG. Safety and COVID-19 Symptoms in Individuals Recently Vaccinated with BCG: a Retrospective Cohort Study. Cell Rep Med. 2020 Aug 25;1(5):100073. doi: 10.1016/j.xcrm.2020.100073. Epub 2020 Aug 5. PMID: 32838341; PMCID: PMC7405881.
https://pubmed.ncbi.nlm.nih.gov/32838341/
186a. Macintyre AN, Gerriets VA, Nichols AG, Michalek RD, Rudolph MC, Deoliveira D, Anderson SM, Abel ED, Chen BJ, Hale LP, Rathmell JC. The glucose transporter Glut1 is selectively essential for CD4 T cell activation and effector function. Cell Metab. 2014 Jul 1;20(1):61-72. doi: 10.1016/j.cmet.2014.05.004. Epub 2014 Jun 12. PMID: 24930970; PMCID: PMC4079750.
https://pubmed.ncbi.nlm.nih.gov/24930970/
186b. Coquillard C, Vilchez V, Marti F, Gedalym R. TOR Signaling in Regulatory T Cell Differentiation and Expansion. SOJ Page 2 of 10 Immunol 3(1): 1-10. DOI: http://dx.doi.org/10.15226/soji/3/1/00122
https://symbiosisonlinepublishing.com/immunology/immunology22.php#
186c. Palmer CS, Palchaudhuri R, Albargy H, Abdel-Mohsen M, Crowe SM. Exploiting immune cell metabolic machinery for functional HIV cure and the prevention of inflammaging. F1000Res. 2018 Jan 30;7:125. doi: 10.12688/f1000research.11881.1. PMID: 29445452; PMCID: PMC5791007.
https://pubmed.ncbi.nlm.nih.gov/29445452/
187. Sa Ribero M, Jouvenet N, Dreux M, Nisole S. Interplay between SARS-CoV-2 and the type I interferon response. PLoS Pathog. 2020 Jul 29;16(7):e1008737. doi: 10.1371/journal.ppat.1008737. PMID: 32726355; PMCID: PMC7390284.
https://pubmed.ncbi.nlm.nih.gov/32726355/
188. Lin F, Shen K. Type I interferon: From innate response to treatment for COVID-19. Pediatr Investig. 2020 Dec 28;4(4):275-280. doi: 10.1002/ped4.12226. PMID: 33376955; PMCID: PMC7768291.
https://pubmed.ncbi.nlm.nih.gov/33376955/
189. Xia H, Shi PY. Antagonism of Type I Interferon by Severe Acute Respiratory Syndrome Coronavirus 2. J Interferon Cytokine Res. 2020 Dec;40(12):543-548. doi: 10.1089/jir.2020.0214. PMID: 33337934; PMCID: PMC7757701.
https://pubmed.ncbi.nlm.nih.gov/33337934/
190. Lopez L, Sang PC, Tian Y, Sang Y. Dysregulated Interferon Response Underlying Severe COVID-19. Viruses. 2020 Dec 13;12(12):1433. doi: 10.3390/v12121433. PMID: 33322160; PMCID: PMC7764122.
https://pubmed.ncbi.nlm.nih.gov/33322160/
191. Suryawanshi RK, Koganti R, Agelidis A, Patil CD, Shukla D. Dysregulation of Cell Signaling by SARS-CoV-2. Trends Microbiol. 2021 Mar;29(3):224-237. doi: 10.1016/j.tim.2020.12.007. Epub 2020 Dec 19. PMID: 33451855; PMCID: PMC7836829
https://pubmed.ncbi.nlm.nih.gov/33451855/
192. Samuel CE. Antiviral actions of interferons. Clin Microbiol Rev. 2001 Oct;14(4):778-809, table of contents. doi: 10.1128/CMR.14.4.778-809.2001. PMID: 11585785; PMCID: PMC89003.
https://pubmed.ncbi.nlm.nih.gov/11585785/
193. Morris R, Kershaw NJ, Babon JJ. The molecular details of cytokine signaling via the JAK/STAT pathway. Protein Sci. 2018 Dec;27(12):1984-2009. doi: 10.1002/pro.3519. PMID: 30267440; PMCID: PMC6237706.
https://pubmed.ncbi.nlm.nih.gov/30267440/
194. Bastard P, Rosen LB, Zhang Q, Michailidis E, Hoffmann HH, Zhang Y, Dorgham K, Philippot Q, Rosain J, Béziat V, Manry J, Shaw E, Haljasmägi L, Peterson P, Lorenzo L, Bizien L, Trouillet-Assant S, Dobbs K, de Jesus AA, Belot A, Kallaste A, Catherinot E, Tandjaoui-Lambiotte Y, Le Pen J, Kerner G, Bigio B, Seeleuthner Y, Yang R, Bolze A, Spaan AN, Delmonte OM, Abers MS, Aiuti A, Casari G, Lampasona V, Piemonti L, Ciceri F, Bilguvar K, Lifton RP, Vasse M, Smadja DM, Migaud M, Hadjadj J, Terrier B, Duffy D, Quintana-Murci L, van de Beek D, Roussel L, Vinh DC, Tangye SG, Haerynck F, Dalmau D, Martinez-Picado J, Brodin P, Nussenzweig MC, Boisson-Dupuis S, Rodríguez-Gallego C, Vogt G, Mogensen TH, Oler AJ, Gu J, Burbelo PD, Cohen JI, Biondi A, Bettini LR, D'Angio M, Bonfanti P, Rossignol P, Mayaux J, Rieux-Laucat F, Husebye ES, Fusco F, Ursini MV, Imberti L, Sottini A, Paghera S, Quiros-Roldan E, Rossi C, Castagnoli R, Montagna D, Licari A, Marseglia GL, Duval X, Ghosn J; HGID Lab; NIAID-USUHS Immune Response to COVID Group; COVID Clinicians; COVID-STORM Clinicians; Imagine COVID Group; French COVID Cohort Study Group; Milieu Intérieur Consortium; CoV-Contact Cohort; Amsterdam UMC Covid-19 Biobank; COVID Human Genetic Effort, Tsang JS, Goldbach-Mansky R, Kisand K, Lionakis MS, Puel A, Zhang SY, Holland SM, Gorochov G, Jouanguy E, Rice CM, Cobat A, Notarangelo LD, Abel L, Su HC, Casanova JL. Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science. 2020 Oct 23;370(6515):eabd4585. doi: 10.1126/science.abd4585. Epub 2020 Sep 24. PMID: 32972996; PMCID: PMC7857397.
https://pubmed.ncbi.nlm.nih.gov/32972996/
195. Meffre E, Iwasaki A. Interferon deficiency can lead to severe COVID. Nature. 2020 Nov;587(7834):374-376. doi: 10.1038/d41586-020-03070-1. PMID: 33139913.
https://pubmed.ncbi.nlm.nih.gov/33139913/
196. Dotan A, Muller S, Kanduc D, David P, Halpert G, Shoenfeld Y. The SARS-CoV-2 as an instrumental trigger of autoimmunity. Autoimmun Rev. 2021 Apr;20(4):102792. doi: 10.1016/j.autrev.2021.102792. Epub 2021 Feb 19. PMID: 33610751; PMCID: PMC7892316.
https://pubmed.ncbi.nlm.nih.gov/33610751/
196a. Khamsi R. Rogue antibodies could be driving severe COVID-19. Nature. 2021 Feb;590(7844):29-31. doi: 10.1038/d41586-021-00149-1. PMID: 33469204.
https://pubmed.ncbi.nlm.nih.gov/33469204/
196b. Ehrenfeld M, Tincani A, Andreoli L, Cattalini M, Greenbaum A, Kanduc D, Alijotas-Reig J, Zinserling V, Semenova N, Amital H, Shoenfeld Y. Covid-19 and autoimmunity. Autoimmun Rev. 2020 Aug;19(8):102597. doi: 10.1016/j.autrev.2020.102597. Epub 2020 Jun 11. PMID: 32535093; PMCID: PMC7289100.
https://pubmed.ncbi.nlm.nih.gov/32535093/
197. Aricò E, Bracci L, Castiello L, Gessani S, Belardelli F. Are we fully exploiting type I Interferons in today's fight against COVID-19 pandemic? Cytokine Growth Factor Rev. 2020 Aug;54:43-50. doi: 10.1016/j.cytogfr.2020.07.010. Epub 2020 Jul 4. PMID: 32665127; PMCID: PMC7334951.
https://pubmed.ncbi.nlm.nih.gov/32665127/
198. Lee JS, Shin EC. The type I interferon response in COVID-19: implications for treatment. Nat Rev Immunol. 2020 Oct;20(10):585-586. doi: 10.1038/s41577-020-00429-3. PMID: 32788708.
https://pubmed.ncbi.nlm.nih.gov/32788708/
199. Zhou Q, Chen V, Shannon CP, Wei XS, Xiang X, Wang X, Wang ZH, Tebbutt SJ, Kollmann TR, Fish EN. Interferon-α2b Treatment for COVID-19. Front Immunol. 2020 May 15;11:1061. doi: 10.3389/fimmu.2020.01061. Erratum in: Front Immunol. 2020 Oct 27;11:615275. PMID: 32574262; PMCID: PMC7242746.
https://pubmed.ncbi.nlm.nih.gov/32574262/
200. Lin F, Shen K. Type I interferon: From innate response to treatment for COVID-19. Pediatr Investig. 2020 Dec 28;4(4):275-280. doi: 10.1002/ped4.12226. PMID: 33376955; PMCID: PMC7768291.
https://pubmed.ncbi.nlm.nih.gov/33376955/
201. Johnson HM, Lewin AS, Ahmed CM. SOCS, Intrinsic Virulence Factors, and Treatment of COVID-19. Front Immunol. 2020 Oct 23;11:582102. doi: 10.3389/fimmu.2020.582102. PMID: 33193390; PMCID: PMC7644869.
https://pubmed.ncbi.nlm.nih.gov/33193390/
202. Liu S, Yan R, Chen B, Pan Q, Chen Y, Hong J, Zhang L, Liu W, Wang S, Chen JL. Influenza Virus-Induced Robust Expression of SOCS3 Contributes to Excessive Production of IL-6. Front Immunol. 2019 Aug 16;10:1843. doi: 10.3389/fimmu.2019.01843. PMID: 31474976; PMCID: PMC6706793.
https://pubmed.ncbi.nlm.nih.gov/31474976/
203. Alti D, Sambamurthy C, Kalangi SK. Emergence of Leptin in Infection and Immunity: Scope and Challenges in Vaccines Formulation. Front Cell Infect Microbiol. 2018 May 9;8:147. doi: 10.3389/fcimb.2018.00147. PMID: 29868503; PMCID: PMC5954041.
https://pubmed.ncbi.nlm.nih.gov/29868503/
204. Akhtar LN, Benveniste EN. Viral exploitation of host SOCS protein functions. J Virol. 2011 Mar;85(5):1912-21. doi: 10.1128/JVI.01857-10. Epub 2010 Nov 17. PMID: 21084484; PMCID: PMC3067810.
https://pubmed.ncbi.nlm.nih.gov/21084484/
205. He B, Tran JT, Sanchez DJ. Manipulation of Type I Interferon Signaling by HIV and AIDS-Associated Viruses. J Immunol Res. 2019 Apr 4;2019:8685312. doi: 10.1155/2019/8685312. PMID: 31089479; PMCID: PMC6476103.
https://pubmed.ncbi.nlm.nih.gov/31089479/
206. Gao W, Hou M, Liu X, Li Z, Yang Y, Zhang W. Induction of SOCS Expression by EV71 Infection Promotes EV71 Replication. Biomed Res Int. 2020 Feb 19;2020:2430640. doi: 10.1155/2020/2430640. PMID: 32149091; PMCID: PMC7054758.
https://pubmed.ncbi.nlm.nih.gov/32149091/
207. Huang S, Liu K, Cheng A, Wang M, Cui M, Huang J, Zhu D, Chen S, Liu M, Zhao X, Wu Y, Yang Q, Zhang S, Ou X, Mao S, Gao Q, Yu Y, Tian B, Liu Y, Zhang L, Yin Z, Jing B, Chen X, Jia R. SOCS Proteins Participate in the Regulation of Innate Immune Response Caused by Viruses. Front Immunol. 2020 Sep 25;11:558341. doi: 10.3389/fimmu.2020.558341. PMID: 33072096; PMCID: PMC7544739.
https://pubmed.ncbi.nlm.nih.gov/33072096/
208. Xie J, Wang M, Cheng A, Jia R, Zhu D, Liu M, Chen S, Zhao X, Yang Q, Wu Y, Zhang S, Luo Q, Wang Y, Xu Z, Chen Z, Zhu L, Liu Y, Yu Y, Zhang L, Chen X. The role of SOCS proteins in the development of virus- induced hepatocellular carcinoma. Virol J. 2021 Apr 13;18(1):74. doi: 10.1186/s12985-021-01544-w. PMID: 33849568; PMCID: PMC8045357.
https://pubmed.ncbi.nlm.nih.gov/33849568/
209. Duncan SA, Baganizi DR, Sahu R, Singh SR, Dennis VA. SOCS Proteins as Regulators of Inflammatory Responses Induced by Bacterial Infections: A Review. Front Microbiol. 2017 Dec 12;8:2431. doi: 10.3389/fmicb.2017.02431. PMID: 29312162; PMCID: PMC5733031.
https://pubmed.ncbi.nlm.nih.gov/29312162/
210. Kindler E, Thiel V. SARS-CoV and IFN: Too Little, Too Late. Cell Host Microbe. 2016 Feb 10;19(2):139-41. doi: 10.1016/j.chom.2016.01.012. PMID: 26867172; PMCID: PMC7104995.
https://pubmed.ncbi.nlm.nih.gov/26867172/
211. Terán-Cabanillas E, Hernández J. Role of Leptin and SOCS3 in Inhibiting the Type I Interferon Response During Obesity. Inflammation. 2017 Feb;40(1):58-67. doi: 10.1007/s10753-016-0452-x. PMID: 27704310.
https://pubmed.ncbi.nlm.nih.gov/27704310/
212. Mahase E. Covid-19: Why are age and obesity risk factors for serious disease? BMJ. 2020 Oct 26;371:m4130. doi: 10.1136/bmj.m4130. PMID: 33106243.
https://pubmed.ncbi.nlm.nih.gov/33106243/
213. Yang A, Guduguntla LS, Yang B. Potentials of Interferons and Hydroxychloroquine for the Prophylaxis and Early Treatment of COVID-19. J Cell Immunol. 2020;2(6):333-340. doi: 10.33696/immunology.2.063. PMID: 33426541; PMCID: PMC7793568.
https://pubmed.ncbi.nlm.nih.gov/33426541/
214. Mudd PA, Crawford JC, Turner JS, Souquette A, Reynolds D, Bender D, Bosanquet JP, Anand NJ, Striker DA, Martin RS, Boon ACM, House SL, Remy KE, Hotchkiss RS, Presti RM, O'Halloran JA, Powderly WG, Thomas PG, Ellebedy AH. Distinct inflammatory profiles distinguish COVID-19 from influenza with limited contributions from cytokine storm. Sci Adv. 2020 Dec 9;6(50):eabe3024. doi: 10.1126/sciadv.abe3024. PMID: 33187979; PMCID: PMC7725462.
https://pubmed.ncbi.nlm.nih.gov/33187979/
215. Hadjadj J, Yatim N, Barnabei L, Corneau A, Boussier J, Smith N, Péré H, Charbit B, Bondet V, Chenevier-Gobeaux C, Breillat P, Carlier N, Gauzit R, Morbieu C, Pène F, Marin N, Roche N, Szwebel TA, Merkling SH, Treluyer JM, Veyer D, Mouthon L, Blanc C, Tharaux PL, Rozenberg F, Fischer A, Duffy D, Rieux-Laucat F, Kernéis S, Terrier B. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science. 2020 Aug 7;369(6504):718-724. doi: 10.1126/science.abc6027. Epub 2020 Jul 13. PMID: 32661059; PMCID: PMC7402632.
https://pubmed.ncbi.nlm.nih.gov/32661059/
216. Jamilloux Y, Henry T, Belot A, Viel S, Fauter M, El Jammal T, Walzer T, François B, Sève P. Should we stimulate or suppress immune responses in COVID-19? Cytokine and anti-cytokine interventions. Autoimmun Rev. 2020 Jul;19(7):102567. doi: 10.1016/j.autrev.2020.102567. Epub 2020 May 4. PMID: 32376392; PMCID: PMC7196557.
https://pubmed.ncbi.nlm.nih.gov/32376392/
217. Onomoto K, Onoguchi K, Yoneyama M. Regulation of RIG-I-like receptor-mediated signaling: interaction between host and viral factors. Cell Mol Immunol. 2021 Mar;18(3):539-555. doi: 10.1038/s41423-020-00602-7. Epub 2021 Jan 18. PMID: 33462384; PMCID: PMC7812568.
https://pubmed.ncbi.nlm.nih.gov/33462384/
218. Mathew D, Giles JR, Baxter AE, Oldridge DA, Greenplate AR, Wu JE, Alanio C, Kuri-Cervantes L, Pampena MB, D'Andrea K, Manne S, Chen Z, Huang YJ, Reilly JP, Weisman AR, Ittner CAG, Kuthuru O, Dougherty J, Nzingha K, Han N, Kim J, Pattekar A, Goodwin EC, Anderson EM, Weirick ME, Gouma S, Arevalo CP, Bolton MJ, Chen F, Lacey SF, Ramage H, Cherry S, Hensley SE, Apostolidis SA, Huang AC, Vella LA; UPenn COVID Processing Unit, Betts MR, Meyer NJ, Wherry EJ. Deep immune profiling of COVID-19 patients reveals distinct immunotypes with therapeutic implications. Science. 2020 Sep 4;369(6508):eabc8511. doi: 10.1126/science.abc8511. Epub 2020 Jul 15. PMID: 32669297; PMCID: PMC7402624.
https://pubmed.ncbi.nlm.nih.gov/32669297/
219. Leviton A, Dammann O. Coagulation, inflammation, and the risk of neonatal white matter damage. Pediatr Res. 2004 Apr;55(4):541-5. doi: 10.1203/01.PDR.0000121197.24154.82. Epub 2004 Feb 18. PMID: 14973176.
https://pubmed.ncbi.nlm.nih.gov/14973176/
220. Esmon CT. The interactions between inflammation and coagulation. Br J Haematol. 2005 Nov;131(4):417-30. doi: 10.1111/j.1365-2141.2005.05753.x. PMID: 16281932.
https://pubmed.ncbi.nlm.nih.gov/16281932/
221. Mosevoll KA, Johansen S, Wendelbo Ø, Nepstad I, Bruserud Ø, Reikvam H. Cytokines, Adhesion Molecules, and Matrix Metalloproteases as Predisposing, Diagnostic, and Prognostic Factors in Venous Thrombosis. Front Med (Lausanne). 2018 May 22;5:147. doi: 10.3389/fmed.2018.00147. PMID: 29872658; PMCID: PMC5972295.
https://pubmed.ncbi.nlm.nih.gov/29872658/
222. Levi M, van der Poll T. Inflammation and coagulation. Crit Care Med. 2010 Feb;38(2 Suppl):S26-34. doi: 10.1097/CCM.0b013e3181c98d21. PMID: 20083910.
https://pubmed.ncbi.nlm.nih.gov/20083910/
223. Budnik I, Brill A. Immune Factors in Deep Vein Thrombosis Initiation. Trends Immunol. 2018 Aug;39(8):610-623. doi: 10.1016/j.it.2018.04.010. Epub 2018 May 16. PMID: 29776849; PMCID: PMC6065414.
https://pubmed.ncbi.nlm.nih.gov/29776849/
224. Iba T, Levy JH, Levi M, Thachil J. Coagulopathy in COVID-19. J Thromb Haemost. 2020 Sep;18(9):2103-2109. doi: 10.1111/jth.14975. Epub 2020 Jul 21. PMID: 32558075; PMCID: PMC7323352.
https://pubmed.ncbi.nlm.nih.gov/32558075/
225. Loof TG, Mörgelin M, Johansson L, Oehmcke S, Olin AI, Dickneite G, Norrby-Teglund A, Theopold U, Herwald H. Coagulation, an ancestral serine protease cascade, exerts a novel function in early immune defense. Blood. 2011 Sep 1;118(9):2589-98. doi: 10.1182/blood-2011-02-337568. Epub 2011 May 25. PMID: 21613262.
https://pubmed.ncbi.nlm.nih.gov/21613262/
226. Rapkiewicz AV, Mai X, Carsons SE, Pittaluga S, Kleiner DE, Berger JS, Thomas S, Adler NM, Charytan DM, Gasmi B, Hochman JS, Reynolds HR. Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: A case series. EClinicalMedicine. 2020 Jun 25;24:100434. doi: 10.1016/j.eclinm.2020.100434. PMID: 32766543; PMCID: PMC7316051.
https://pubmed.ncbi.nlm.nih.gov/32766543/
227. Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy Brown J, Vander Heide RS. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med. 2020 Jul;8(7):681-686. doi: 10.1016/S2213-2600(20)30243-5. Epub 2020 May 27. PMID: 32473124; PMCID: PMC7255143.
https://pubmed.ncbi.nlm.nih.gov/32473124/
228. Wichmann D, Sperhake JP, Lütgehetmann M, Steurer S, Edler C, Heinemann A, Heinrich F, Mushumba H, Kniep I, Schröder AS, Burdelski C, de Heer G, Nierhaus A, Frings D, Pfefferle S, Becker H, Bredereke-Wiedling H, de Weerth A, Paschen HR, Sheikhzadeh-Eggers S, Stang A, Schmiedel S, Bokemeyer C, Addo MM, Aepfelbacher M, Püschel K, Kluge S. Autopsy Findings and Venous Thromboembolism in Patients With COVID-19: A Prospective Cohort Study. Ann Intern Med. 2020 Aug 18;173(4):268-277. doi: 10.7326/M20-2003. Epub 2020 May 6. PMID: 32374815; PMCID: PMC7240772.
https://pubmed.ncbi.nlm.nih.gov/32374815/
229. Belen-Apak FB, Sarıalioğlu F. Pulmonary intravascular coagulation in COVID-19: possible pathogenesis and recommendations on anticoagulant/thrombolytic therapy. J Thromb Thrombolysis. 2020 Aug;50(2):278-280. doi: 10.1007/s11239-020-02129-0. PMID: 32372336; PMCID: PMC7200048.
https://pubmed.ncbi.nlm.nih.gov/32372336/
230. Zhang AJ, To KK, Li C, Lau CC, Poon VK, Chan CC, Zheng BJ, Hung IF, Lam KS, Xu A, Yuen KY. Leptin mediates the pathogenesis of severe 2009 pandemic influenza A(H1N1) infection associated with cytokine dysregulation in mice with diet-induced obesity. J Infect Dis. 2013 Apr 15;207(8):1270-80. doi: 10.1093/infdis/jit031. Epub 2013 Jan 16. PMID: 23325916.
https://pubmed.ncbi.nlm.nih.gov/23325916/
231. La Cava A, Matarese G. The weight of leptin in immunity. Nat Rev Immunol. 2004 May;4(5):371-9. doi: 10.1038/nri1350. PMID: 15122202.
https://pubmed.ncbi.nlm.nih.gov/15122202/
232. Cohen S, Danzaki K, MacIver NJ. Nutritional effects on T-cell immunometabolism. Eur J Immunol. 2017 Feb;47(2):225-235. doi: 10.1002/eji.201646423. Epub 2017 Jan 24. PMID: 28054344; PMCID: PMC5342627.
https://pubmed.ncbi.nlm.nih.gov/28054344/
233. Fischer HJ, Sie C, Schumann E, Witte AK, Dressel R, van den Brandt J, Reichardt HM. The Insulin Receptor Plays a Critical Role in T Cell Function and Adaptive Immunity. J Immunol. 2017 Mar 1;198(5):1910-1920. doi: 10.4049/jimmunol.1601011. Epub 2017 Jan 23. PMID: 28115529.
https://pubmed.ncbi.nlm.nih.gov/28115529/
234. Tsai S, Clemente-Casares X, Zhou AC, Lei H, Ahn JJ, Chan YT, Choi O, Luck H, Woo M, Dunn SE, Engleman EG, Watts TH, Winer S, Winer DA. Insulin Receptor-Mediated Stimulation Boosts T Cell Immunity during Inflammation and Infection. Cell Metab. 2018 Dec 4;28(6):922-934.e4. doi: 10.1016/j.cmet.2018.08.003. Epub 2018 Aug 30. PMID: 30174303.
https://pubmed.ncbi.nlm.nih.gov/30174303/
235. Lagunas-Rangel FA. Neutrophil-to-lymphocyte ratio and lymphocyte-to-C-reactive protein ratio in patients with severe coronavirus disease 2019 (COVID-19): A meta-analysis. J Med Virol. 2020 Oct;92(10):1733-1734. doi: 10.1002/jmv.25819. Epub 2020 Apr 8. PMID: 32242950; PMCID: PMC7228336.
https://pubmed.ncbi.nlm.nih.gov/32242950/
236. Li X, Liu C, Mao Z, Xiao M, Wang L, Qi S, Zhou F. Predictive values of neutrophil-to-lymphocyte ratio on disease severity and mortality in COVID-19 patients: a systematic review and meta-analysis. Crit Care. 2020 Nov 16;24(1):647. doi: 10.1186/s13054-020-03374-8. PMID: 33198786; PMCID: PMC7667659.
https://pubmed.ncbi.nlm.nih.gov/33198786/
237. Piatkiewicz P, Czech A, Tatoń J. Glucose transport in human peripheral blood lymphocytes influenced by type 2 diabetes mellitus. Arch Immunol Ther Exp (Warsz). 2007 Mar-Apr;55(2):119-26. doi: 10.1007/s00005-007-0015-9. Epub 2007 Mar 20. PMID: 17417692; PMCID: PMC2765645.
https://pubmed.ncbi.nlm.nih.gov/17417692/
238. Ieronymaki E, Theodorakis EM, Lyroni K, Vergadi E, Lagoudaki E, Al-Qahtani A, Aznaourova M, Neofotistou-Themeli E, Eliopoulos AG, Vaporidi K, Tsatsanis C. Insulin Resistance in Macrophages Alters Their Metabolism and Promotes an M2-Like Phenotype. J Immunol. 2019 Mar 15;202(6):1786-1797. doi: 10.4049/jimmunol.1800065. Epub 2019 Feb 4. PMID: 30718296.
https://pubmed.ncbi.nlm.nih.gov/30718296/
239. Cunnane SC, Trushina E, Morland C, Prigione A, Casadesus G, Andrews ZB, Beal MF, Bergersen LH, Brinton RD, de la Monte S, Eckert A, Harvey J, Jeggo R, Jhamandas JH, Kann O, la Cour CM, Martin WF, Mithieux G, Moreira PI, Murphy MP, Nave KA, Nuriel T, Oliet SHR, Saudou F, Mattson MP, Swerdlow RH, Millan MJ. Brain energy rescue: an emerging therapeutic concept for neurodegenerative disorders of ageing. Nat Rev Drug Discov. 2020 Sep;19(9):609-633. doi: 10.1038/s41573-020-0072-x. Epub 2020 Jul 24. PMID: 32709961; PMCID: PMC7948516.
https://pubmed.ncbi.nlm.nih.gov/32709961/
240. Femminella GD, Livingston NR, Raza S, van der Doef T, Frangou E, Love S, Busza G, Calsolaro V, Carver S, Holmes C, Ritchie CW, Lawrence RM, McFarlane B, Tadros G, Ridha BH, Bannister C, Walker Z, Archer H, Coulthard E, Underwood B, Prasanna A, Koranteng P, Karim S, Junaid K, McGuinness B, Passmore AP, Nilforooshan R, Macharouthu A, Donaldson A, Thacker S, Russell G, Malik N, Mate V, Knight L, Kshemendran S, Tan T, Holscher C, Harrison J, Brooks DJ, Ballard C, Edison P. Does insulin resistance influence neurodegeneration in non-diabetic Alzheimer's subjects? Alzheimers Res Ther. 2021 Feb 17;13(1):47. doi: 10.1186/s13195-021-00784-w. PMID: 33597002; PMCID: PMC7890851.
https://pubmed.ncbi.nlm.nih.gov/33597002/
241. Palmer, Clovis S and S. Crowe. The role of glucose and lipid metabolism in the pathogenesis of HIV-1 infection. Current Trends in Immunology, 13, 37-50.
https://research.monash.edu/en/publications/the-role-of-glucose-and-lipi...
242. Palmer CS, Hussain T, Duette G, Weller TJ, Ostrowski M, Sada-Ovalle I, Crowe SM. Regulators of Glucose Metabolism in CD4+ and CD8+ T Cells. Int Rev Immunol. 2016 Nov;35(6):477-488. doi: 10.3109/08830185.2015.1082178. Epub 2015 Nov 25. PMID: 26606199.
https://pubmed.ncbi.nlm.nih.gov/26606199/
243. Saucillo DC, Gerriets VA, Sheng J, Rathmell JC, Maciver NJ. Leptin metabolically licenses T cells for activation to link nutrition and immunity. J Immunol. 2014 Jan 1;192(1):136-44. doi: 10.4049/jimmunol.1301158. Epub 2013 Nov 22. PMID: 24273001; PMCID: PMC3872216.
https://pubmed.ncbi.nlm.nih.gov/24273001/
244. Pearce EL, Pearce EJ. Metabolic pathways in immune cell activation and quiescence. Immunity. 2013 Apr 18;38(4):633-43. doi: 10.1016/j.immuni.2013.04.005. PMID: 23601682; PMCID: PMC3654249.
https://pubmed.ncbi.nlm.nih.gov/23601682/
245. Koester-Weber T, Valtueña J, Breidenassel C, Beghin L, Plada M, Moreno S, Huybrechts I, Palacios G, Gómez-Martínez S, Albers U, De Henauw S, Maiani G, Kafatos A, Molnar D, Sjöstrom M, Widhalm K, Manios Y, Moreno LA, Marcos A, Castillo MJ, Stehle P, Gonzalez-Gross M. Reference values for leptin, cortisol, insulin and glucose, among European adolescents and their association with adiposity: the HELENA study. Nutr Hosp. 2014 Nov 1;30(5):1181-90. doi: 10.3305/nh.2014.30.5.7982. PMID: 25365025.
https://pubmed.ncbi.nlm.nih.gov/25365025/
245a. van Dielen FM, van't Veer C, Schols AM, Soeters PB, Buurman WA, Greve JW. Increased leptin concentrations correlate with increased concentrations of inflammatory markers in morbidly obese individuals. Int J Obes Relat Metab Disord. 2001 Dec;25(12):1759-66. doi: 10.1038/sj.ijo.0801825. PMID: 11781755.
https://pubmed.ncbi.nlm.nih.gov/11781755/
246. Pérez-Pérez A, Vilariño-García T, Fernández-Riejos P, Martín-González J, Segura-Egea JJ, Sánchez-Margalet V. Role of leptin as a link between metabolism and the immune system. Cytokine Growth Factor Rev. 2017 Jun;35:71-84. doi: 10.1016/j.cytogfr.2017.03.001. Epub 2017 Mar 4. PMID: 28285098.
https://pubmed.ncbi.nlm.nih.gov/28285098/
247. Iikuni N, Lam QL, Lu L, Matarese G, La Cava A. Leptin and Inflammation. Curr Immunol Rev. 2008 May 1;4(2):70-79. doi: 10.2174/157339508784325046. PMID: 20198122; PMCID: PMC2829991.
https://pubmed.ncbi.nlm.nih.gov/20198122/
248. Wang J, Xu Y, Zhang X, Wang S, Peng Z, Guo J, Jiang H, Liu J, Xie Y, Wang J, Li X, Liao J, Wan C, Yu L, Hu J, Liu B, Liu Z. Leptin correlates with monocytes activation and severe condition in COVID-19 patients. J Leukoc Biol. 2021 Jan 6. doi: 10.1002/JLB.5HI1020-704R. Epub ahead of print. PMID: 33404078.
https://pubmed.ncbi.nlm.nih.gov/33404078/
249. Recchiuti A. As a matter of fat: Leptin, monocyte hyperactivation, and COVID-19: A commentary to "Leptin correlates with monocytes activation and severe condition in COVID-19 patients". J Leukoc Biol. 2021 Apr 13. doi: 10.1002/JLB.3CE1220-799R. Epub ahead of print. PMID: 33847393.
https://pubmed.ncbi.nlm.nih.gov/33847393/
250. Naylor C, Petri WA Jr. Leptin Regulation of Immune Responses. Trends Mol Med. 2016 Feb;22(2):88-98. doi: 10.1016/j.molmed.2015.12.001. Epub 2016 Jan 14. PMID: 26776093.
https://pubmed.ncbi.nlm.nih.gov/26776093/
251. Mantzoros CS, Magkos F, Brinkoetter M, Sienkiewicz E, Dardeno TA, Kim SY, Hamnvik OP, Koniaris A. Leptin in human physiology and pathophysiology. Am J Physiol Endocrinol Metab. 2011 Oct;301(4):E567-84. doi: 10.1152/ajpendo.00315.2011. Epub 2011 Jul 26. PMID: 21791620; PMCID: PMC3191548.
https://pubmed.ncbi.nlm.nih.gov/21791620/
252. Pérez-Pérez A, Sánchez-Jiménez F, Vilariño-García T, Sánchez-Margalet V. Role of Leptin in Inflammation and Vice Versa. Int J Mol Sci. 2020 Aug 16;21(16):5887. doi: 10.3390/ijms21165887. PMID: 32824322; PMCID: PMC7460646.
https://pubmed.ncbi.nlm.nih.gov/32824322/
253. Chen W, Daines MO, Khurana Hershey GK. Turning off signal transducer and activator of transcription (STAT): the negative regulation of STAT signaling. J Allergy Clin Immunol. 2004 Sep;114(3):476-89; quiz 490. doi: 10.1016/j.jaci.2004.06.042. PMID: 15356544.
https://pubmed.ncbi.nlm.nih.gov/15356544/
254. Andersen CJ, Murphy KE, Fernandez ML. Impact of Obesity and Metabolic Syndrome on Immunity. Adv Nutr. 2016 Jan 15;7(1):66-75. doi: 10.3945/an.115.010207. PMID: 26773015; PMCID: PMC4717890.
https://pubmed.ncbi.nlm.nih.gov/26773015/
255. Hur SJ, Kim DH, Chun SC, Lee SK. Effect of adenovirus and influenza virus infection on obesity. Life Sci. 2013 Oct 11;93(16):531-5. doi: 10.1016/j.lfs.2013.08.016. Epub 2013 Sep 2. PMID: 24007799.
https://pubmed.ncbi.nlm.nih.gov/24007799/
256. Popkin BM, Du S, Green WD, Beck MA, Algaith T, Herbst CH, Alsukait RF, Alluhidan M, Alazemi N, Shekar M. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes Rev. 2020 Nov;21(11):e13128. doi: 10.1111/obr.13128. Epub 2020 Aug 26. PMID: 32845580; PMCID: PMC7461480.
https://pubmed.ncbi.nlm.nih.gov/32845580/
257. Drucker DJ. Diabetes, obesity, metabolism, and SARS-CoV-2 infection: the end of the beginning. Cell Metab. 2021 Mar 2;33(3):479-498. doi: 10.1016/j.cmet.2021.01.016. Epub 2021 Jan 21. PMID: 33529600; PMCID: PMC7825982.
https://pubmed.ncbi.nlm.nih.gov/33529600/
258. Zakka K, Chidambaram S, Mansour S, Mahawar K, Salminen P, Almino R, Schauer P, Kinross J, Purkayastha S; PanSurg Collaborative. SARS-CoV-2 and Obesity: "CoVesity"-a Pandemic Within a Pandemic. Obes Surg. 2021 Apr;31(4):1745-1754. doi: 10.1007/s11695-020-04919-0. Epub 2021 Jan 22. PMID: 33479921; PMCID: PMC7819768.
https://pubmed.ncbi.nlm.nih.gov/33479921/
259. Aguilar EG, Murphy WJ. Obesity induced T cell dysfunction and implications for cancer immunotherapy. Curr Opin Immunol. 2018 Apr;51:181-186. doi: 10.1016/j.coi.2018.03.012. Epub 2018 Apr 11. PMID: 29655021; PMCID: PMC6338436.
https://pubmed.ncbi.nlm.nih.gov/29655021/
260. Aiello A, Farzaneh F, Candore G, Caruso C, Davinelli S, Gambino CM, Ligotti ME, Zareian N, Accardi G. Immunosenescence and Its Hallmarks: How to Oppose Aging Strategically? A Review of Potential Options for Therapeutic Intervention. Front Immunol. 2019 Sep 25;10:2247. doi: 10.3389/fimmu.2019.02247. PMID: 31608061; PMCID: PMC6773825.
https://pubmed.ncbi.nlm.nih.gov/31608061/
261. Stefan N, Birkenfeld AL, Schulze MB. Global pandemics interconnected - obesity, impaired metabolic health and COVID-19. Nat Rev Endocrinol. 2021 Mar;17(3):135-149. doi: 10.1038/s41574-020-00462-1. Epub 2021 Jan 21. PMID: 33479538.
https://pubmed.ncbi.nlm.nih.gov/33479538/
262. Pawelec G. Age and immunity: What is "immunosenescence"? Exp Gerontol. 2018 May;105:4-9. doi: 10.1016/j.exger.2017.10.024. Epub 2017 Oct 27. PMID: 29111233.
https://pubmed.ncbi.nlm.nih.gov/29111233/
263. Pawelec G. The human immunosenescence phenotype: does it exist? Semin Immunopathol. 2020 Oct;42(5):537-544. doi: 10.1007/s00281-020-00810-3. Epub 2020 Aug 5. PMID: 32757035; PMCID: PMC7405710.
https://pubmed.ncbi.nlm.nih.gov/32757035/
264. Pawelec G, Bronikowski A, Cunnane SC, Ferrucci L, Franceschi C, Fülöp T, Gaudreau P, Gladyshev VN, Gonos ES, Gorbunova V, Kennedy BK, Larbi A, Lemaître JF, Liu GH, Maier AB, Morais JA, Nóbrega OT, Moskalev A, Rikkert MO, Seluanov A, Senior AM, Ukraintseva S, Vanhaelen Q, Witkowski J, Cohen AA. The conundrum of human immune system "senescence". Mech Ageing Dev. 2020 Dec;192:111357. doi: 10.1016/j.mad.2020.111357. Epub 2020 Sep 17. PMID: 32949594; PMCID: PMC7494491.
https://pubmed.ncbi.nlm.nih.gov/32949594/
265. Steven S, Hollingsworth KG, Al-Mrabeh A, Avery L, Aribisala B, Caslake M, Taylor R. Very Low-Calorie Diet and 6 Months of Weight Stability in Type 2 Diabetes: Pathophysiological Changes in Responders and Nonresponders. Diabetes Care. 2016 May;39(5):808-15. doi: 10.2337/dc15-1942. Epub 2016 Mar 21. Erratum in: Diabetes Care. 2018 Apr 24;: PMID: 27002059.
https://pubmed.ncbi.nlm.nih.gov/27002059/
265a. Pot GK, Battjes-Fries MC, Patijn ON, Pijl H, Witkamp RF, de Visser M, van der Zijl N, de Vries M, Voshol PJ. Nutrition and lifestyle intervention in type 2 diabetes: pilot study in the Netherlands showing improved glucose control and reduction in glucose lowering medication. BMJ Nutr Prev Health. 2019 May 14;2(1):43-50. doi: 10.1136/bmjnph-2018-000012. PMID: 33235957; PMCID: PMC7678479.
https://pubmed.ncbi.nlm.nih.gov/33235957/
266. Appari M, Channon KM, McNeill E. Metabolic Regulation of Adipose Tissue Macrophage Function in Obesity and Diabetes. Antioxid Redox Signal. 2018 Jul 20;29(3):297-312. doi: 10.1089/ars.2017.7060. Epub 2017 Oct 13. PMID: 28661198; PMCID: PMC6012981.
https://pubmed.ncbi.nlm.nih.gov/28661198/
267. Tanti JF, Ceppo F, Jager J, Berthou F. Implication of inflammatory signaling pathways in obesity-induced insulin resistance. Front Endocrinol (Lausanne). 2013 Jan 8;3:181. doi: 10.3389/fendo.2012.00181. PMID: 23316186; PMCID: PMC3539134.
https://pubmed.ncbi.nlm.nih.gov/23316186/
268. Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. 1993 Jan 1;259(5091):87-91. doi: 10.1126/science.7678183. PMID: 7678183.
https://pubmed.ncbi.nlm.nih.gov/7678183/
269. Ouchi N, Parker JL, Lugus JJ, Walsh K. Adipokines in inflammation and metabolic disease. Nat Rev Immunol. 2011 Feb;11(2):85-97. doi: 10.1038/nri2921. Epub 2011 Jan 21. PMID: 21252989; PMCID: PMC3518031.
https://pubmed.ncbi.nlm.nih.gov/21252989/
270. Mancuso P. The role of adipokines in chronic inflammation. Immunotargets Ther. 2016 May 23;5:47-56. doi: 10.2147/ITT.S73223. PMID: 27529061; PMCID: PMC4970637.
https://pubmed.ncbi.nlm.nih.gov/27529061/
271. Lepsch J, Farias DR, Vaz Jdos S, de Jesus Pereira Pinto T, da Silva Lima N, Freitas Vilela AA, Cunha M, Factor-Litvak P, Kac G. Serum saturated fatty acid decreases plasma adiponectin and increases leptin throughout pregnancy independently of BMI. Nutrition. 2016 Jul-Aug;32(7-8):740-7. doi: 10.1016/j.nut.2016.01.016. Epub 2016 Jan 30. PMID: 27036610.
https://pubmed.ncbi.nlm.nih.gov/27036610/
272. Cole SA, Laviada-Molina HA, Serres-Perales JM, Rodriguez-Ayala E, Bastarrachea RA. The COVID-19 Pandemic during the Time of the Diabetes Pandemic: Likely Fraternal Twins? Pathogens. 2020 May 19;9(5):389. doi: 10.3390/pathogens9050389. PMID: 32438687; PMCID: PMC7281197.
https://pubmed.ncbi.nlm.nih.gov/32438687/
273. Sudhakaran M, Doseff AI. The Targeted Impact of Flavones on Obesity-Induced Inflammation and the Potential Synergistic Role in Cancer and the Gut Microbiota. Molecules. 2020 May 27;25(11):2477. doi: 10.3390/molecules25112477. PMID: 32471061; PMCID: PMC7321129.
https://pubmed.ncbi.nlm.nih.gov/32471061/
273a. Cole SA, Laviada-Molina HA, Serres-Perales JM, Rodriguez-Ayala E, Bastarrachea RA. The COVID-19 Pandemic during the Time of the Diabetes Pandemic: Likely Fraternal Twins? Pathogens. 2020 May 19;9(5):389. doi: 10.3390/pathogens9050389. PMID: 32438687; PMCID: PMC7281197.
https://pubmed.ncbi.nlm.nih.gov/32438687/
274. Ganji V, Kafai MR, McCarthy E. Serum leptin concentrations are not related to dietary patterns but are related to sex, age, body mass index, serum triacylglycerol, serum insulin, and plasma glucose in the US population. Nutr Metab (Lond). 2009 Jan 14;6:3. doi: 10.1186/1743-7075-6-3. PMID: 19144201; PMCID: PMC2657130.
https://pubmed.ncbi.nlm.nih.gov/19144201/
275. Gijón-Conde T, Graciani A, Guallar-Castillón P, Aguilera MT, Rodríguez-Artalejo F, Banegas JR. Leptin Reference Values and Cutoffs for Identifying Cardiometabolic Abnormalities in the Spanish Population. Rev Esp Cardiol (Engl Ed). 2015 Aug;68(8):672-9. doi: 10.1016/j.rec.2014.08.015. Epub 2015 Jan 22. PMID: 25618563.
https://pubmed.ncbi.nlm.nih.gov/25618563/
276. Andreoli MF, Donato J, Cakir I, Perello M. Leptin resensitisation: a reversion of leptin-resistant states. J Endocrinol. 2019 Jun 1;241(3):R81-R96. doi: 10.1530/JOE-18-0606. PMID: 30959481.
https://pubmed.ncbi.nlm.nih.gov/30959481/
277. Hadden DR, McLaughlin C. Normal and abnormal maternal metabolism during pregnancy. Semin Fetal Neonatal Med. 2009 Apr;14(2):66-71. doi: 10.1016/j.siny.2008.09.004. Epub 2008 Nov 4. Erratum in: Semin Fetal Neonatal Med. 2009 Dec;14(6):401. PMID: 18986856.
https://pubmed.ncbi.nlm.nih.gov/18986856/
278. Könner AC, Brüning JC. Selective insulin and leptin resistance in metabolic disorders. Cell Metab. 2012 Aug 8;16(2):144-52. doi: 10.1016/j.cmet.2012.07.004. PMID: 22883229.
https://pubmed.ncbi.nlm.nih.gov/22883229/
279. Zhao S, Zhu Y, Schultz RD, Li N, He Z, Zhang Z, Caron A, Zhu Q, Sun K, Xiong W, Deng H, Sun J, Deng Y, Kim M, Lee CE, Gordillo R, Liu T, Odle AK, Childs GV, Zhang N, Kusminski CM, Elmquist JK, Williams KW, An Z, Scherer PE. Partial Leptin Reduction as an Insulin Sensitization and Weight Loss Strategy. Cell Metab. 2019 Oct 1;30(4):706-719.e6. doi: 10.1016/j.cmet.2019.08.005. Epub 2019 Sep 5. PMID: 31495688; PMCID: PMC6774814.
https://pubmed.ncbi.nlm.nih.gov/31495688/
280. LeRoith D. Beta-cell dysfunction and insulin resistance in type 2 diabetes: role of metabolic and genetic abnormalities. Am J Med. 2002 Oct 28;113 Suppl 6A:3S-11S. doi: 10.1016/s0002-9343(02)01276-7. PMID: 12431757.
https://pubmed.ncbi.nlm.nih.gov/12431757/
281. Stefan N, Birkenfeld AL, Schulze MB. Global pandemics interconnected - obesity, impaired metabolic health and COVID-19. Nat Rev Endocrinol. 2021 Mar;17(3):135-149. doi: 10.1038/s41574-020-00462-1. Epub 2021 Jan 21. PMID: 33479538.
https://pubmed.ncbi.nlm.nih.gov/33479538/
282. Wang S, Ma P, Zhang S, Song S, Wang Z, Ma Y, Xu J, Wu F, Duan L, Yin Z, Luo H, Xiong N, Xu M, Zeng T, Jin Y. Fasting blood glucose at admission is an independent predictor for 28-day mortality in patients with COVID-19 without previous diagnosis of diabetes: a multi-centre retrospective study. Diabetologia. 2020 Oct;63(10):2102-2111. doi: 10.1007/s00125-020-05209-1. Epub 2020 Jul 10. PMID: 32647915; PMCID: PMC7347402.
https://pubmed.ncbi.nlm.nih.gov/32647915/
283. Tucker ME. Hyperglycemia Predicts COVID-19 Death Even Without Diabetes. Medscape 13 July 2020. Accessed 21 April 2021.
https://www.medscape.com/viewarticle/933787
284. Cai Y, Shi S, Yang F, Yi B, Chen X, Li J, Wen Z. Fasting blood glucose level is a predictor of mortality in patients with COVID-19 independent of diabetes history. Diabetes Res Clin Pract. 2020 Nov;169:108437. doi: 10.1016/j.diabres.2020.108437. Epub 2020 Sep 10. PMID: 32920103; PMCID: PMC7482587.
https://pubmed.ncbi.nlm.nih.gov/32920103/
285. Shanmugam N, Reddy MA, Guha M, Natarajan R. High glucose-induced expression of proinflammatory cytokine and chemokine genes in monocytic cells. Diabetes. 2003 May;52(5):1256-64. doi: 10.2337/diabetes.52.5.1256. PMID: 12716761.
https://pubmed.ncbi.nlm.nih.gov/12716761/
286. Dandona P, Chaudhuri A, Ghanim H, Mohanty P. Proinflammatory effects of glucose and anti-inflammatory effect of insulin: relevance to cardiovascular disease. Am J Cardiol. 2007 Feb 19;99(4A):15B-26B. doi: 10.1016/j.amjcard.2006.11.003. Epub 2006 Dec 27. PMID: 17307055.
https://pubmed.ncbi.nlm.nih.gov/17307055/
287. Fardini Y, Dehennaut V, Lefebvre T, Issad T. O-GlcNAcylation: A New Cancer Hallmark? Front Endocrinol (Lausanne). 2013 Aug 12;4:99. doi: 10.3389/fendo.2013.00099. PMID: 23964270; PMCID: PMC3740238.
https://pubmed.ncbi.nlm.nih.gov/23964270/
288. Wang Q, Fang P, He R, Li M, Yu H, Zhou L, Yi Y, Wang F, Rong Y, Zhang Y, Chen A, Peng N, Lin Y, Lu M, Zhu Y, Peng G, Rao L, Liu S. O-GlcNAc transferase promotes influenza A virus-induced cytokine storm by targeting interferon regulatory factor-5. Sci Adv. 2020 Apr 15;6(16):eaaz7086. doi: 10.1126/sciadv.aaz7086. PMID: 32494619; PMCID: PMC7159909.
https://pubmed.ncbi.nlm.nih.gov/32494619/
289. Williams R. Discovered: Metabolic Mechanism of Cytokine Storms. The Scientist Magazine_April 2020. Accessed 21 April 2021.
https://www.the-scientist.com/news-opinion/discovered-metabolic-mechanis...
290. Codo AC, Davanzo GG, Monteiro LB, de Souza GF, Muraro SP, Virgilio-da-Silva JV, Prodonoff JS, Carregari VC, de Biagi Junior CAO, Crunfli F, Jimenez Restrepo JL, Vendramini PH, Reis-de-Oliveira G, Bispo Dos Santos K, Toledo-Teixeira DA, Parise PL, Martini MC, Marques RE, Carmo HR, Borin A, Coimbra LD, Boldrini VO, Brunetti NS, Vieira AS, Mansour E, Ulaf RG, Bernardes AF, Nunes TA, Ribeiro LC, Palma AC, Agrela MV, Moretti ML, Sposito AC, Pereira FB, Velloso LA, Vinolo MAR, Damasio A, Proença-Módena JL, Carvalho RF, Mori MA, Martins-de-Souza D, Nakaya HI, Farias AS, Moraes-Vieira PM. Elevated Glucose Levels Favor SARS-CoV-2 Infection and Monocyte Response through a HIF-1α/Glycolysis-Dependent Axis. Cell Metab. 2020 Sep 1;32(3):437-446.e5. doi: 10.1016/j.cmet.2020.07.007. Epub 2020 Jul 17. Erratum in: Cell Metab. 2020 Sep 1;32(3):498-499. PMID: 32697943; PMCID: PMC7367032.
https://pubmed.ncbi.nlm.nih.gov/32697943/
291. Thompson CD, Matta B, Barnes BJ. Therapeutic Targeting of IRFs: Pathway-Dependence or Structure-Based? Front Immunol. 2018 Nov 20;9:2622. doi: 10.3389/fimmu.2018.02622. PMID: 30515152; PMCID: PMC6255967.
https://pubmed.ncbi.nlm.nih.gov/30515152/
292. Alzaid F, Julla JB, Diedisheim M, Potier C, Potier L, Velho G, Gaborit B, Manivet P, Germain S, Vidal-Trecan T, Roussel R, Riveline JP, Dalmas E, Venteclef N, Gautier JF. Monocytopenia, monocyte morphological anomalies and hyperinflammation characterise severe COVID-19 in type 2 diabetes. EMBO Mol Med. 2020 Oct 7;12(10):e13038. doi: 10.15252/emmm.202013038. Epub 2020 Sep 11. PMID: 32816392; PMCID: PMC7461002.
https://pubmed.ncbi.nlm.nih.gov/32816392/
293. Brzeska A, Swidrowska J, Smolewska E. Leptin as an Important Hormone and Immunomodulator in Adult and Childhood Rheumatoid Arthritis. Global Journal of Immunology and Allergic Diseases, 2013, 1, 16-24.
https://www.researchgate.net/publication/314946274_Leptin_as_an_Importan...
294. Abella V, Scotece M, Conde J, Pino J, Gonzalez-Gay MA, Gómez-Reino JJ, Mera A, Lago F, Gómez R, Gualillo O. Leptin in the interplay of inflammation, metabolism and immune system disorders. Nat Rev Rheumatol. 2017 Feb;13(2):100-109. doi: 10.1038/nrrheum.2016.209. Epub 2017 Jan 5. PMID: 28053336.
https://pubmed.ncbi.nlm.nih.gov/28053336/
295. de Candia P, Prattichizzo F, Garavelli S, Alviggi C, La Cava A, Matarese G. The pleiotropic roles of leptin in metabolism, immunity, and cancer. J Exp Med. 2021 May 3;218(5):e20191593. doi: 10.1084/jem.20191593. PMID: 33857282.
https://pubmed.ncbi.nlm.nih.gov/33857282/
295a. Fernández-Riejos P, Najib S, Santos-Alvarez J, Martín-Romero C, Pérez-Pérez A, González-Yanes C, Sánchez-Margalet V. Role of leptin in the activation of immune cells. Mediators Inflamm. 2010;2010:568343. doi: 10.1155/2010/568343. Epub 2010 Mar 23. PMID: 20368778; PMCID: PMC2846344.
https://pubmed.ncbi.nlm.nih.gov/20368778/
296. Kiernan K, MacIver NJ. The Role of the Adipokine Leptin in Immune Cell Function in Health and Disease. Front Immunol. 2021 Jan 29;11:622468. doi: 10.3389/fimmu.2020.622468. PMID: 33584724; PMCID: PMC7878386.
https://pubmed.ncbi.nlm.nih.gov/33584724/
297. Lee J, Liu J, Feng X, Salazar Hernández MA, Mucka P, Ibi D, Choi JW, Ozcan U. Withaferin A is a leptin sensitizer with strong antidiabetic properties in mice. Nat Med. 2016 Sep;22(9):1023-32. doi: 10.1038/nm.4145. Epub 2016 Aug 1. PMID: 27479085; PMCID: PMC5892415.
https://pubmed.ncbi.nlm.nih.gov/27479085/
298. Münzberg H, Flier JS, Bjørbaek C. Region-specific leptin resistance within the hypothalamus of diet-induced obese mice. Endocrinology. 2004 Nov;145(11):4880-9. doi: 10.1210/en.2004-0726. Epub 2004 Jul 22. PMID: 15271881.
https://pubmed.ncbi.nlm.nih.gov/15271881/
299. Howard JK, Flier JS. Attenuation of leptin and insulin signaling by SOCS proteins. Trends Endocrinol Metab. 2006 Nov;17(9):365-71. doi: 10.1016/j.tem.2006.09.007. Epub 2006 Sep 28. PMID: 17010638.
https://pubmed.ncbi.nlm.nih.gov/17010638/
300. Ueki K, Kondo T, Kahn CR. Suppressor of cytokine signaling 1 (SOCS-1) and SOCS-3 cause insulin resistance through inhibition of tyrosine phosphorylation of insulin receptor substrate proteins by discrete mechanisms. Mol Cell Biol. 2004 Jun;24(12):5434-46. doi: 10.1128/MCB.24.12.5434-5446.2004. Erratum in: Mol Cell Biol. 2005 Oct;25(19):8762. PMID: 15169905; PMCID: PMC419873.
https://pubmed.ncbi.nlm.nih.gov/15169905/
301. Ernst MB, Wunderlich CM, Hess S, Paehler M, Mesaros A, Koralov SB, Kleinridders A, Husch A, Münzberg H, Hampel B, Alber J, Kloppenburg P, Brüning JC, Wunderlich FT. Enhanced Stat3 activation in POMC neurons provokes negative feedback inhibition of leptin and insulin signaling in obesity. J Neurosci. 2009 Sep 16;29(37):11582-93. doi: 10.1523/JNEUROSCI.5712-08.2009. PMID: 19759305; PMCID: PMC6665760.
https://pubmed.ncbi.nlm.nih.gov/19759305/
302. Yang Z, Hulver M, McMillan RP, Cai L, Kershaw EE, Yu L, Xue B, Shi H. Regulation of insulin and leptin signaling by muscle suppressor of cytokine signaling 3 (SOCS3). PLoS One. 2012;7(10):e47493. doi: 10.1371/journal.pone.0047493. Epub 2012 Oct 24. PMID: 23115649; PMCID: PMC3480378.
https://pubmed.ncbi.nlm.nih.gov/23115649/
303. Wunderlich CM, Hövelmeyer N, Wunderlich FT. Mechanisms of chronic JAK-STAT3-SOCS3 signaling in obesity. JAKSTAT. 2013 Apr 1;2(2):e23878. doi: 10.4161/jkst.23878. PMID: 24058813; PMCID: PMC3710326.
https://pubmed.ncbi.nlm.nih.gov/24058813/
304. Carow B, Rottenberg ME. SOCS3, a Major Regulator of Infection and Inflammation. Front Immunol. 2014 Feb 19;5:58. doi: 10.3389/fimmu.2014.00058. PMID: 24600449; PMCID: PMC3928676.
https://pubmed.ncbi.nlm.nih.gov/24600449/
305. Zhou D, Chen L, Yang K, Jiang H, Xu W, Luan J. SOCS molecules: the growing players in macrophage polarization and function. Oncotarget. 2017 Aug 4;8(36):60710-60722. doi: 10.18632/oncotarget.19940. PMID: 28948005; PMCID: PMC5601173.
https://pubmed.ncbi.nlm.nih.gov/28948005/
306. Pedroso JAB, Ramos-Lobo AM, Donato J Jr. SOCS3 as a future target to treat metabolic disorders. Hormones (Athens). 2019 Jun;18(2):127-136. doi: 10.1007/s42000-018-0078-5. Epub 2018 Nov 9. PMID: 30414080.
https://pubmed.ncbi.nlm.nih.gov/30414080/
307. Dey S, Murmu N, Bose M, Ghosh S, Giri B. Obesity and chronic leptin resistance foster insulin resistance: An analytical overview. BLDE Univ J Health Sci 2021;6:7-21
https://www.bldeujournalhs.in/article.asp?issn=2468-838X;year=2021;volum...
308. Warren KJ, Olson MM, Thompson NJ, Cahill ML, Wyatt TA, Yoon KJ, Loiacono CM, Kohut ML. Exercise Improves Host Response to Influenza Viral Infection in Obese and Non-Obese Mice through Different Mechanisms. PLoS One. 2015 Jun 25;10(6):e0129713. doi: 10.1371/journal.pone.0129713. PMID: 26110868; PMCID: PMC4482026.
https://pubmed.ncbi.nlm.nih.gov/26110868/
309. Zheng Q, Cui G, Chen J, Gao H, Wei Y, Uede T, Chen Z, Diao H. Regular Exercise Enhances the Immune Response Against Microbial Antigens Through Up-Regulation of Toll-like Receptor Signaling Pathways. Cell Physiol Biochem. 2015;37(2):735-46. doi: 10.1159/000430391. Epub 2015 Sep 11. PMID: 26356264.
https://pubmed.ncbi.nlm.nih.gov/26356264/
310. Bouassida A, Zalleg D, Bouassida S, Zaouali M, Feki Y, Zbidi A, Tabka Z. Leptin, its implication in physical exercise and training: a short review. J Sports Sci Med. 2006 Jun 1;5(2):172-81. PMID: 24259989; PMCID: PMC3827558.
https://pubmed.ncbi.nlm.nih.gov/24259989/
311. Yi JS, Cox MA, Zajac AJ. T-cell exhaustion: characteristics, causes and conversion. Immunology. 2010 Apr;129(4):474-81. doi: 10.1111/j.1365-2567.2010.03255.x. Epub 2010 Feb 23. PMID: 20201977; PMCID: PMC2842494.
https://pubmed.ncbi.nlm.nih.gov/20201977/
312. Wherry EJ. T cell exhaustion. Nat Immunol. 2011 Jun;12(6):492-9. doi: 10.1038/ni.2035. PMID: 21739672.
https://pubmed.ncbi.nlm.nih.gov/21739672/
313. Blank CU, Haining WN, Held W, Hogan PG, Kallies A, Lugli E, Lynn RC, Philip M, Rao A, Restifo NP, Schietinger A, Schumacher TN, Schwartzberg PL, Sharpe AH, Speiser DE, Wherry EJ, Youngblood BA, Zehn D. Defining 'T cell exhaustion'. Nat Rev Immunol. 2019 Nov;19(11):665-674. doi: 10.1038/s41577-019-0221-9. Epub 2019 Sep 30. PMID: 31570879; PMCID: PMC7286441.
https://pubmed.ncbi.nlm.nih.gov/31570879/
314. Kahan SM, Zajac AJ. Immune Exhaustion: Past Lessons and New Insights from Lymphocytic Choriomeningitis Virus. Viruses. 2019 Feb 13;11(2):156. doi: 10.3390/v11020156. PMID: 30781904; PMCID: PMC6410286.
https://pubmed.ncbi.nlm.nih.gov/30781904/
315. Diao B, Wang C, Tan Y, Chen X, Liu Y, Ning L, Chen L, Li M, Liu Y, Wang G, Yuan Z, Feng Z, Zhang Y, Wu Y, Chen Y. Reduction and Functional Exhaustion of T Cells in Patients With Coronavirus Disease 2019 (COVID-19). Front Immunol. 2020 May 1;11:827. doi: 10.3389/fimmu.2020.00827. PMID: 32425950; PMCID: PMC7205903.
https://pubmed.ncbi.nlm.nih.gov/32425950/
316. Paces J, Strizova Z, Smrz D, Cerny J. COVID-19 and the immune system. Physiol Res. 2020 Jul 16;69(3):379-388. doi: 10.33549/physiolres.934492. Epub 2020 May 29. PMID: 32469225.
https://pubmed.ncbi.nlm.nih.gov/32469225/
317. Jordan SC. Innate and adaptive immune responses to SARS-CoV-2 in humans: relevance to acquired immunity and vaccine responses. Clin Exp Immunol. 2021 Feb 3:10.1111/cei.13582. doi: 10.1111/cei.13582. Epub ahead of print. PMID: 33534923; PMCID: PMC8013613.
https://pubmed.ncbi.nlm.nih.gov/33534923/
318. Pawelec G. Age and immunity: What is "immunosenescence"? Exp Gerontol. 2018 May;105:4-9. doi: 10.1016/j.exger.2017.10.024. Epub 2017 Oct 27. PMID: 29111233.
https://pubmed.ncbi.nlm.nih.gov/29111233/
319. Pawelec G. Aging as an inflammatory disease and possible reversal strategies. J Allergy Clin Immunol. 2020 May;145(5):1355-1356. doi: 10.1016/j.jaci.2020.02.022. Epub 2020 Mar 4. PMID: 32142747.
https://pubmed.ncbi.nlm.nih.gov/32142747/
320. Pawelec G. The human immunosenescence phenotype: does it exist? Semin Immunopathol. 2020 Oct;42(5):537-544. doi: 10.1007/s00281-020-00810-3. Epub 2020 Aug 5. PMID: 32757035; PMCID: PMC7405710.
https://pubmed.ncbi.nlm.nih.gov/32757035/
321. Pawelec G, Bronikowski A, Cunnane SC, Ferrucci L, Franceschi C, Fülöp T, Gaudreau P, Gladyshev VN, Gonos ES, Gorbunova V, Kennedy BK, Larbi A, Lemaître JF, Liu GH, Maier AB, Morais JA, Nóbrega OT, Moskalev A, Rikkert MO, Seluanov A, Senior AM, Ukraintseva S, Vanhaelen Q, Witkowski J, Cohen AA. The conundrum of human immune system "senescence". Mech Ageing Dev. 2020 Dec;192:111357. doi: 10.1016/j.mad.2020.111357. Epub 2020 Sep 17. PMID: 32949594; PMCID: PMC7494491.
https://pubmed.ncbi.nlm.nih.gov/32949594/
321a. Bates C.J. (2004) Common Nutrient Deficiencies in Older Adults. In: Bales C.W., Ritchie C.S. (eds) Handbook of Clinical Nutrition and Aging. Nutrition and Health. Humana Press, Totowa, NJ. https://doi.org/10.1007/978-1-59259-391-0_6
https://link.springer.com/chapter/10.1007/978-1-59259-391-0_6#citeas
321b. Vural Z, Avery A, Kalogiros DI, Coneyworth LJ, Welham SJM. Trace Mineral Intake and Deficiencies in Older Adults Living in the Community and Institutions: A Systematic Review. Nutrients. 2020 Apr 13;12(4):1072. doi: 10.3390/nu12041072. PMID: 32294896; PMCID: PMC7230219.
https://pubmed.ncbi.nlm.nih.gov/32294896/
322. Pae M, Meydani SN, Wu D. The role of nutrition in enhancing immunity in aging. Aging Dis. 2012 Feb;3(1):91-129. Epub 2011 Sep 30. PMID: 22500273; PMCID: PMC3320807.
https://pubmed.ncbi.nlm.nih.gov/22500273/
323. Pae M, Wu D. Nutritional modulation of age-related changes in the immune system and risk of infection. Nutr Res. 2017 May;41:14-35. doi: 10.1016/j.nutres.2017.02.001. Epub 2017 Feb 4. PMID: 28577789.
https://pubmed.ncbi.nlm.nih.gov/28577789/
324. Ivory K, Prieto E, Spinks C, Armah CN, Goldson AJ, Dainty JR, Nicoletti C. Selenium supplementation has beneficial and detrimental effects on immunity to influenza vaccine in older adults. Clin Nutr. 2017 Apr;36(2):407-415. doi: 10.1016/j.clnu.2015.12.003. Epub 2015 Dec 24. PMID: 26803169; PMCID: PMC5381341.
https://pubmed.ncbi.nlm.nih.gov/26803169/
325. Maggini S, Pierre A, Calder PC. Immune Function and Micronutrient Requirements Change over the Life Course. Nutrients. 2018 Oct 17;10(10):1531. doi: 10.3390/nu10101531. PMID: 30336639; PMCID: PMC6212925.
https://pubmed.ncbi.nlm.nih.gov/30336639/
326. Torrinhas RS, Calder PC, Lemos GO, Waitzberg DL. Parenteral fish oil: An adjuvant pharmacotherapy for coronavirus disease 2019? Nutrition. 2021 Jan;81:110900. doi: 10.1016/j.nut.2020.110900. Epub 2020 Jun 20. PMID: 32738510; PMCID: PMC7836308.
https://pubmed.ncbi.nlm.nih.gov/32738510/
327. Yang H, Youm YH, Vandanmagsar B, Rood J, Kumar KG, Butler AA, Dixit VD. Obesity accelerates thymic aging. Blood. 2009 Oct 29;114(18):3803-12. doi: 10.1182/blood-2009-03-213595. Epub 2009 Aug 31. PMID: 19721009; PMCID: PMC2773495.
https://pubmed.ncbi.nlm.nih.gov/19721009/
328. Suri S. The efficacy of COVID19 vaccines is linked to good nutrition. ORF Observer Research Foundation, Health Express 1 March 2021, Accessed 22 Aprl 2021
https://www.orfonline.org/expert-speak/the-efficacy-of-covid19-vaccines-....
329. Zimmermann P, Curtis N. Factors That Influence the Immune Response to Vaccination. Clin Microbiol Rev. 2019 Mar 13;32(2):e00084-18. doi: 10.1128/CMR.00084-18. PMID: 30867162; PMCID: PMC6431125.
https://pubmed.ncbi.nlm.nih.gov/30867162/
330. Alhadi MA, Friedman LM, Karlsson EA, Cohen-Lavi L, Burkovitz A, Schultz-Cherry S, Noah TL, Weir SS, Shulman LM, Beck MA, Hertz T. Obesity is associated with an altered baseline and post-vaccination influenza antibody repertoire. medRxiv [Preprint]. 2021 Mar 5:2021.03.02.21252785. doi: 10.1101/2021.03.02.21252785. PMID: 33688682; PMCID: PMC7941659.
https://pubmed.ncbi.nlm.nih.gov/33688682/
331. Lindeberg S, Söderberg S, Ahrén B, Olsson T. Large differences in serum leptin levels between nonwesternized and westernized populations: the Kitava study. J Intern Med. 2001 Jun;249(6):553-8. doi: 10.1046/j.1365-2796.2001.00845.x. PMID: 11422662.