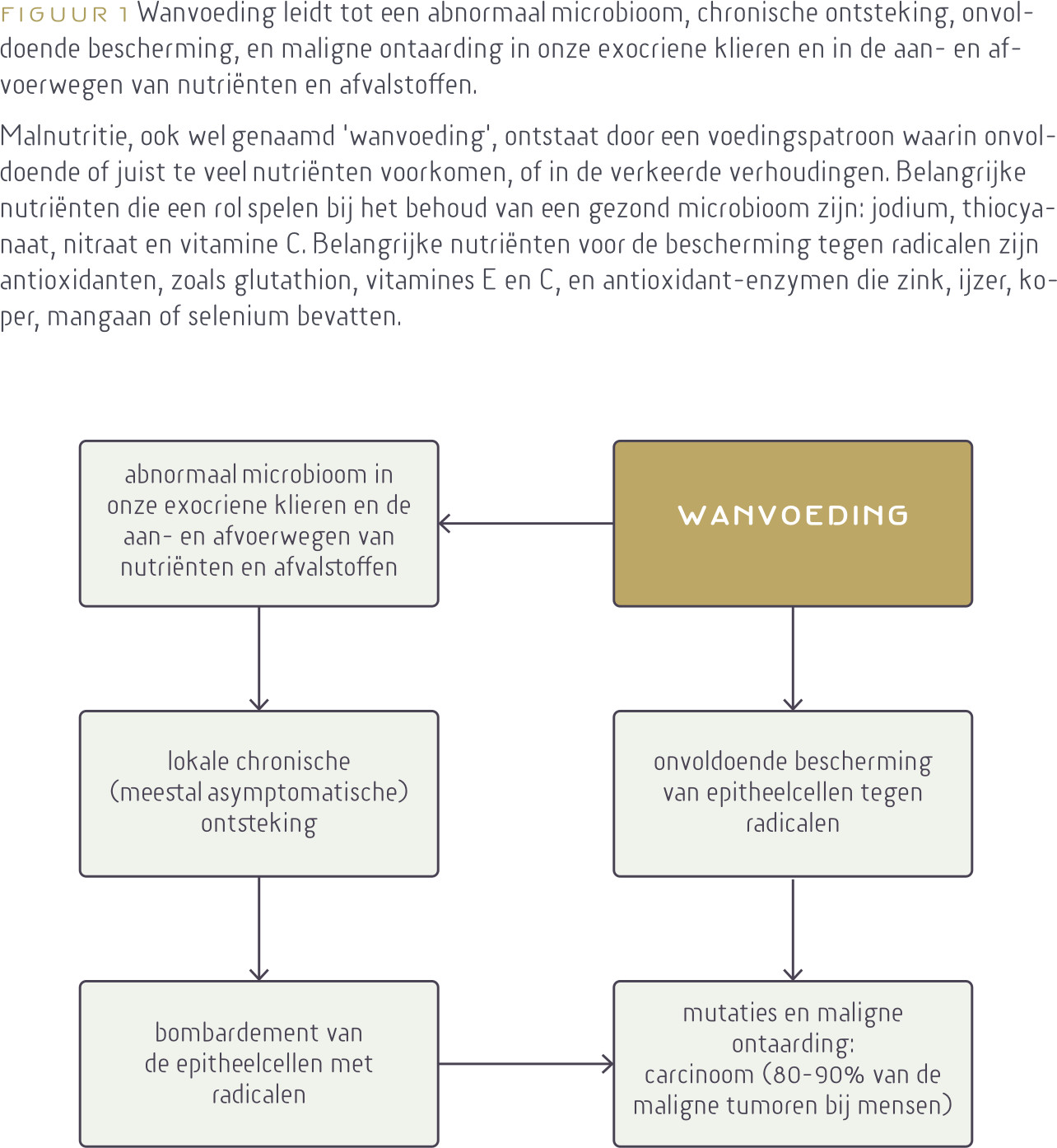
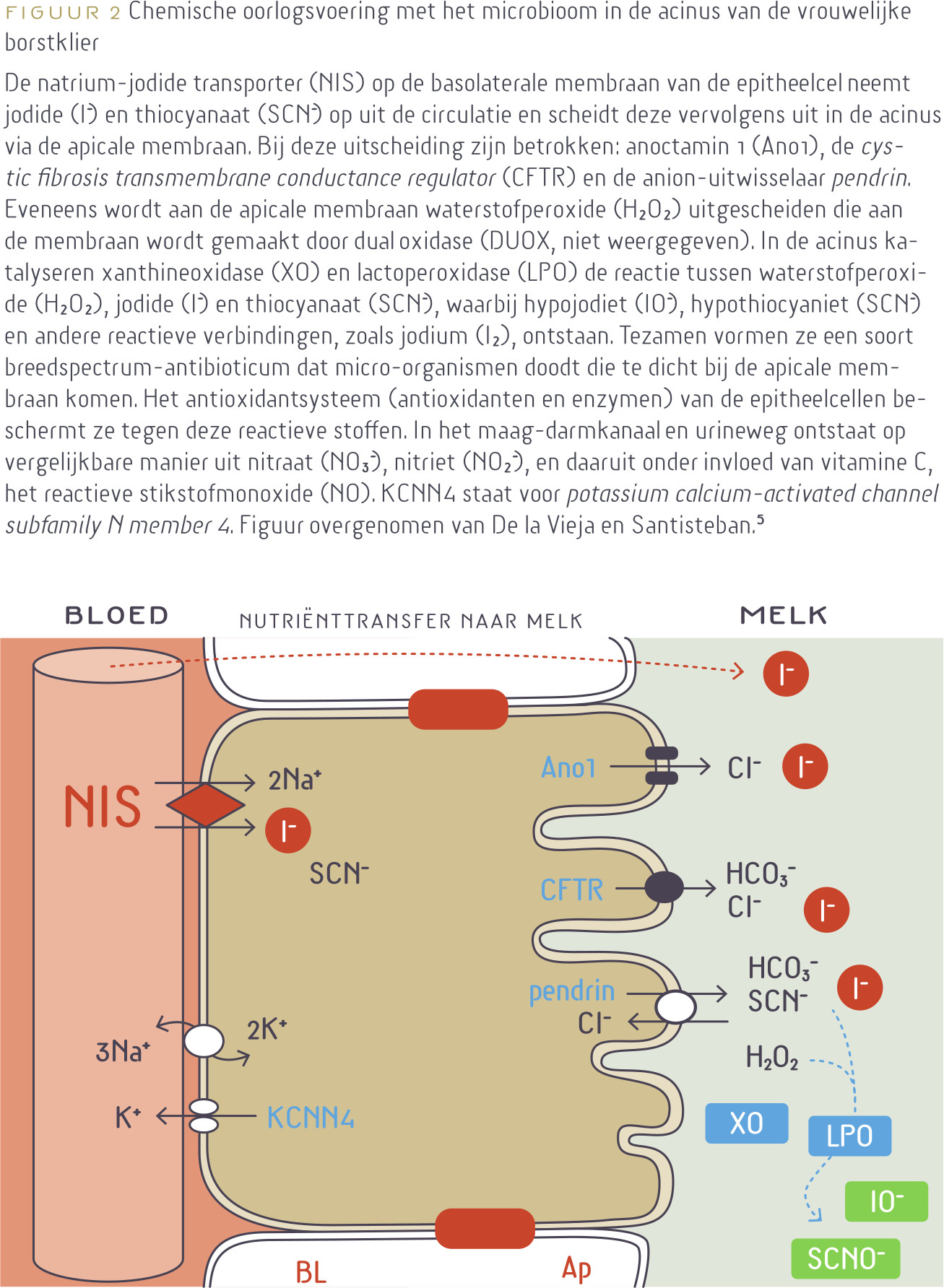
Via onze huid, luchtwegen, maag-darmkanaal en urineweg grenzen we aan een vijandige omgeving. Deze bestaat onder andere uit microben, zoals parasieten, bacteriën, schimmels en virussen, die ons maar wat graag als feestmaal willen benutten. Deels treffen ze een solide barrière, zoals in het grootste deel van de huid, maar in de longen, maag-darmkanaal en de nieren kunnen we niet anders dan met de omgeving communiceren vanwege de (terug)opname van voedingsstoffen en zuurstof, en de uitscheiding van afval, waaronder ureum, kooldioxide (CO2) enzovoort. Op die plaatsen vindt een ware strijd plaats met microben onder regie van ons immuunsysteem dat zich daarvoor onder andere bedient van chemische oorlogsvoering. Voor deze strijd zijn onderdelen nodig voor de productie van munitie in de vorm van talrijke nutriënten, waaronder nitraat,1-3 jodium,4-6 thiocyanaat,5,7,8 selenium6,9,10 en vitamine C.1-3,11
Beste bezoeker, u heeft geen toegang.
Enkel (web)abonnees hebben toegang tot tijdschriftartikelen. Het webabonnement is nog in de maak.
U kunt zich wel alvast (gratis) registreren en tal van andere webartikelen raadplegen!
Auteur
Verschenen in
Referenties
1. Hord NG, Tang Y, Bryan NS. Food sources of nitrates and nitrites: the physiologic context for potential health benefits. Am J Clin Nutr. 2009 Jul;90(1):1-10. doi: 10.3945/ajcn.2008.27131. Epub 2009 May 13. PMID: 19439460.
https://pubmed.ncbi.nlm.nih.gov/19439460/
2. Bryan NS, Ahmed S, Lefer DJ, Hord N, von Schwarz ER. Dietary nitrate biochemistry and physiology. An update on clinical benefits and mechanisms of action. Nitric Oxide. 2023 Mar 1;132:1-7. doi: 10.1016/j.niox.2023.01.003. Epub 2023 Jan 20. PMID: 36690137.
https://pubmed.ncbi.nlm.nih.gov/36690137/
3. Du J, Filipović MR, Wagner BA, Buettner GR. Ascorbate mediates the non-enzymatic reduction of nitrite to nitric oxide. Adv Redox Res. 2023 Dec;9:100079. doi: 10.1016/j.arres.2023.100079. Epub 2023 Aug 15. PMID: 37692975; PMCID: PMC10486277.
https://pubmed.ncbi.nlm.nih.gov/37692975/
4. Fuge, R. (2012). Soils and iodine deficiency. In Essentials of medical geology: revised edition (pp. 417-432). Dordrecht: Springer Netherlands.
https://link.springer.com/chapter/10.1007/978-94-007-4375-5_17
5. De la Vieja A, Santisteban P. Role of iodide metabolism in physiology and cancer. Endocr Relat Cancer. 2018 Apr;25(4):R225-R245. doi: 10.1530/ERC-17-0515. Epub 2018 Feb 1. PMID: 29437784.
https://pubmed.ncbi.nlm.nih.gov/29437784/
6. Dijck-Brouwer DAJ, Muskiet FAJ, Verheesen RH, Schaafsma G, Schaafsma A, Geurts JMW. Thyroidal and Extrathyroidal Requirements for Iodine and Selenium: A Combined Evolutionary and (Patho)Physiological Approach. Nutrients. 2022 Sep 20;14(19):3886. doi: 10.3390/nu14193886. PMID: 36235539; PMCID: PMC9571367.
https://pubmed.ncbi.nlm.nih.gov/36235539/
7. Patel U, Gingerich A, Widman L, Sarr D, Tripp RA, Rada B. Susceptibility of influenza viruses to hypothiocyanite and hypoiodite produced by lactoperoxidase in a cell-free system. PLoS One. 2018 Jul 25;13(7):e0199167. doi: 10.1371/journal.pone.0199167. PMID: 30044776; PMCID: PMC6059396.
https://pubmed.ncbi.nlm.nih.gov/30044776/
8. Bafort F, Parisi O, Perraudin JP, Jijakli MH. Mode of action of lactoperoxidase as related to its antimicrobial activity: a review. Enzyme Res. 2014;2014:517164. doi: 10.1155/2014/517164. Epub 2014 Sep 16. PMID: 25309750; PMCID: PMC4182067.
https://pubmed.ncbi.nlm.nih.gov/25309750/
9. Fordyce, F. M. (2012). Selenium deficiency and toxicity in the environment. In Essentials of medical geology: Revised edition (pp. 375-416). Dordrecht: Springer Netherlands.
https://link.springer.com/chapter/10.1007/978-94-007-4375-5_16
10. Schomburg L. Selenium Deficiency Due to Diet, Pregnancy, Severe Illness, or COVID-19-A Preventable Trigger for Autoimmune Disease. Int J Mol Sci. 2021 Aug 8;22(16):8532. doi: 10.3390/ijms22168532. PMID: 34445238; PMCID: PMC8395178.
https://pubmed.ncbi.nlm.nih.gov/34445238/
11. Padayatty SJ, Levine M. Vitamin C: the known and the unknown and Goldilocks. Oral Dis. 2016 Sep;22(6):463-93. doi: 10.1111/odi.12446. Epub 2016 Apr 14. PMID: 26808119; PMCID: PMC4959991.
https://pubmed.ncbi.nlm.nih.gov/26808119/
12. Urbaniak C, Cummins J, Brackstone M, Macklaim JM, Gloor GB, Baban CK, Scott L, O'Hanlon DM, Burton JP, Francis KP, Tangney M, Reid G. Microbiota of human breast tissue. Appl Environ Microbiol. 2014 May;80(10):3007-14. doi: 10.1128/AEM.00242-14. Epub 2014 Mar 7. PMID: 24610844; PMCID: PMC4018903.
https://pubmed.ncbi.nlm.nih.gov/24610844/
13. Latuga MS, Stuebe A, Seed PC. A review of the source and function of microbiota in breast milk. Semin Reprod Med. 2014 Jan;32(1):68-73. doi: 10.1055/s-0033-1361824. Epub 2014 Jan 3. PMID: 24390923.
https://pubmed.ncbi.nlm.nih.gov/24390923/
14. Walker WA, Iyengar RS. Breast milk, microbiota, and intestinal immune homeostasis. Pediatr Res. 2015 Jan;77(1-2):220-8. doi: 10.1038/pr.2014.160. Epub 2014 Oct 13. PMID: 25310762.
https://pubmed.ncbi.nlm.nih.gov/25310762/
15. Eslami-S Z, Majidzadeh-A K, Halvaei S, Babapirali F, Esmaeili R. Microbiome and Breast Cancer: New Role for an Ancient Population. Front Oncol. 2020 Feb 12;10:120. doi: 10.3389/fonc.2020.00120. PMID: 32117767; PMCID: PMC7028701.
https://pubmed.ncbi.nlm.nih.gov/32117767/
16. Kim SY, Yi DY. Components of human breast milk: from macronutrient to microbiome and microRNA. Clin Exp Pediatr. 2020 Aug;63(8):301-309. doi: 10.3345/cep.2020.00059. Epub 2020 Mar 23. PMID: 32252145; PMCID: PMC7402982.
https://pubmed.ncbi.nlm.nih.gov/32252145/
17. Laborda-Illanes A, Sanchez-Alcoholado L, Dominguez-Recio ME, Jimenez-Rodriguez B, Lavado R, Comino-Méndez I, Alba E, Queipo-Ortuño MI. Breast and Gut Microbiota Action Mechanisms in Breast Cancer Pathogenesis and Treatment. Cancers (Basel). 2020 Aug 31;12(9):2465. doi: 10.3390/cancers12092465. PMID: 32878124; PMCID: PMC7565530.
https://pubmed.ncbi.nlm.nih.gov/32878124/
18. Tzeng A, Sangwan N, Jia M, Liu CC, Keslar KS, Downs-Kelly E, Fairchild RL, Al-Hilli Z, Grobmyer SR, Eng C. Human breast microbiome correlates with prognostic features and immunological signatures in breast cancer. Genome Med. 2021 Apr 16;13(1):60. doi: 10.1186/s13073-021-00874-2. PMID: 33863341; PMCID: PMC8052771.
https://pubmed.ncbi.nlm.nih.gov/33863341/
19. Dieleman S, Aarnoutse R, Ziemons J, Kooreman L, Boleij A, Smidt M. Exploring the Potential of Breast Microbiota as Biomarker for Breast Cancer and Therapeutic Response. Am J Pathol. 2021 Jun;191(6):968-982. doi: 10.1016/j.ajpath.2021.02.020. Epub 2021 Mar 10. PMID: 33713687.
https://pubmed.ncbi.nlm.nih.gov/33713687/
20. Toumazi D, El Daccache S, Constantinou C. An unexpected link: The role of mammary and gut microbiota on breast cancer development and management (Review). Oncol Rep. 2021 May;45(5):80. doi: 10.3892/or.2021.8031. Epub 2021 Mar 31. PMID: 33786630.
https://pubmed.ncbi.nlm.nih.gov/33786630/
21. Feng ZP, Xin HY, Zhang ZW, Liu CG, Yang Z, You H, Xin HW. Gut microbiota homeostasis restoration may become a novel therapy for breast cancer. Invest New Drugs. 2021 Jun;39(3):871-878. doi: 10.1007/s10637-021-01063-z. Epub 2021 Jan 17. PMID: 33454868.
https://pubmed.ncbi.nlm.nih.gov/33454868/
22. Wu H, Ganguly S, Tollefsbol TO. Modulating Microbiota as a New Strategy for Breast Cancer Prevention and Treatment. Microorganisms. 2022 Aug 27;10(9):1727. doi: 10.3390/microorganisms10091727. PMID: 36144329; PMCID: PMC9503838.
https://pubmed.ncbi.nlm.nih.gov/36144329/
23. Thu MS, Chotirosniramit K, Nopsopon T, Hirankarn N, Pongpirul K. Human gut, breast, and oral microbiome in breast cancer: A systematic review and meta-analysis. Front Oncol. 2023 Mar 17;13:1144021. doi: 10.3389/fonc.2023.1144021. PMID: 37007104; PMCID: PMC10063924.
https://pubmed.ncbi.nlm.nih.gov/37007104/
24. Zheng H, Wang C, Yu X, Zheng W, An Y, Zhang J, Zhang Y, Wang G, Qi M, Lin H, Wang F. The Role of Metabolomics and Microbiology in Urinary Tract Infection. Int J Mol Sci. 2024 Mar 8;25(6):3134. doi: 10.3390/ijms25063134. PMID: 38542107; PMCID: PMC10969911.
https://pubmed.ncbi.nlm.nih.gov/38542107/
25. Kustrimovic N, Bombelli R, Baci D, Mortara L. Microbiome and Prostate Cancer: A Novel Target for Prevention and Treatment. Int J Mol Sci. 2023 Jan 12;24(2):1511. doi: 10.3390/ijms24021511. PMID: 36675055; PMCID: PMC9860633.
https://pubmed.ncbi.nlm.nih.gov/36675055/
26. Anderson SM, Sears CL. The Role of the Gut Microbiome in Cancer: A Review, With Special Focus on Colorectal Neoplasia and Clostridioides difficile. Clin Infect Dis. 2023 Dec 5;77(Suppl 6):S471-S478. doi: 10.1093/cid/ciad640. PMID: 38051969; PMCID: PMC10697667.
https://pubmed.ncbi.nlm.nih.gov/38051969/
27. Spragge F, Bakkeren E, Jahn MT, B N Araujo E, Pearson CF, Wang X, Pankhurst L, Cunrath O, Foster KR. Microbiome diversity protects against pathogens by nutrient blocking. Science. 2023 Dec 15;382(6676):eadj3502. doi: 10.1126/science.adj3502. Epub 2023 Dec 15. PMID: 38096285.
https://pubmed.ncbi.nlm.nih.gov/38096285/
28. Kumar A, Baruah A, Tomioka M, Iino Y, Kalita MC, Khan M. Caenorhabditis elegans: a model to understand host-microbe interactions. Cell Mol Life Sci. 2020 Apr;77(7):1229-1249. doi: 10.1007/s00018-019-03319-7. Epub 2019 Oct 4. PMID: 31584128.
https://pubmed.ncbi.nlm.nih.gov/31584128/
28a. NIH. Cancer Classification
https://training.seer.cancer.gov/disease/categories/classification.html
29. Lowe DB, Storkus WJ. Chronic inflammation and immunologic-based constraints in malignant disease. Immunotherapy. 2011 Oct;3(10):1265-74. doi: 10.2217/imt.11.113. PMID: 21995576; PMCID: PMC3225121.
https://pubmed.ncbi.nlm.nih.gov/21995576/
30. Multhoff G, Molls M, Radons J. Chronic inflammation in cancer development. Front Immunol. 2012 Jan 12;2:98. doi: 10.3389/fimmu.2011.00098. PMID: 22566887; PMCID: PMC3342348.
https://pubmed.ncbi.nlm.nih.gov/22566887/
31. Greten FR, Grivennikov SI. Inflammation and Cancer: Triggers, Mechanisms, and Consequences. Immunity. 2019 Jul 16;51(1):27-41. doi: 10.1016/j.immuni.2019.06.025. PMID: 31315034; PMCID: PMC6831096.
https://pubmed.ncbi.nlm.nih.gov/31315034/
32. Singh N, Baby D, Rajguru JP, Patil PB, Thakkannavar SS, Pujari VB. Inflammation and cancer. Ann Afr Med. 2019 Jul-Sep;18(3):121-126. doi: 10.4103/aam.aam_56_18. PMID: 31417011; PMCID: PMC6704802.
https://pubmed.ncbi.nlm.nih.gov/31417011/
33. Zhao H, Wu L, Yan G, Chen Y, Zhou M, Wu Y, Li Y. Inflammation and tumor progression: signaling pathways and targeted intervention. Signal Transduct Target Ther. 2021 Jul 12;6(1):263. doi: 10.1038/s41392-021-00658-5. PMID: 34248142; PMCID: PMC8273155.
https://pubmed.ncbi.nlm.nih.gov/34248142/
34. Liu X, Yin L, Shen S, Hou Y. Inflammation and cancer: paradoxical roles in tumorigenesis and implications in immunotherapies. Genes Dis. 2021 Oct 18;10(1):151-164. doi: 10.1016/j.gendis.2021.09.006. PMID: 37013041; PMCID: PMC10066281.
https://pubmed.ncbi.nlm.nih.gov/37013041/
35. Rayburn ER, Ezell SJ, Zhang R. Anti-Inflammatory Agents for Cancer Therapy. Mol Cell Pharmacol. 2009;1(1):29-43. doi: 10.4255/mcpharmacol.09.05. PMID: 20333321; PMCID: PMC2843097.
https://pubmed.ncbi.nlm.nih.gov/20333321/
36. Jiang J, Li J, Yunxia Z, Zhu H, Liu J, Pumill C. The role of prostatitis in prostate cancer: meta-analysis. PLoS One. 2013 Dec 31;8(12):e85179. doi: 10.1371/journal.pone.0085179. PMID: 24391995; PMCID: PMC3877315.
https://pubmed.ncbi.nlm.nih.gov/24391995/
37. Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002 Dec 19-26;420(6917):860-7. doi: 10.1038/nature01322. PMID: 12490959; PMCID: PMC2803035.
https://pubmed.ncbi.nlm.nih.gov/12490959/
38. Follin-Arbelet B, Cvancarova Småstuen M, Hovde Ø, Jelsness-Jørgensen LP, Moum B. Risk of Cancer in Patients With Crohn's Disease 30 Years After Diagnosis (the IBSEN Study). Crohns Colitis 360. 2023 Oct 3;5(4):otad057. doi: 10.1093/crocol/otad057. PMID: 37886706; PMCID: PMC10599393.
https://pubmed.ncbi.nlm.nih.gov/37886706/
39. Sun J. Impact of bacterial infection and intestinal microbiome on colorectal cancer development. Chin Med J (Engl). 2022 Jan 27;135(4):400-408. doi: 10.1097/CM9.0000000000001979. PMID: 35089888; PMCID: PMC8869519.
https://pubmed.ncbi.nlm.nih.gov/35089888/
40. Chang CM, Lin MC, Yin WY. Risk of breast cancer in women with non-lactational mastitis. Sci Rep. 2019 Oct 30;9(1):15587. doi: 10.1038/s41598-019-52046-3. PMID: 31666573; PMCID: PMC6821708.
https://pubmed.ncbi.nlm.nih.gov/31666573/
41. Chen YC, Chan CH, Lim YB, Yang SF, Yeh LT, Wang YH, Chou MC, Yeh CB. Risk of Breast Cancer in Women with Mastitis: A Retrospective Population-Based Cohort Study. Medicina (Kaunas). 2020 Jul 24;56(8):372. doi: 10.3390/medicina56080372. PMID: 32722165; PMCID: PMC7466309.
https://pubmed.ncbi.nlm.nih.gov/32722165/
42. Wu C, Zhang Z, Lu Z, Liao M, Zhang Y, Xie Y, Guo X, Yu X, Yang X, Gao Y, Tan A, Mo Z. Prevalence of and risk factors for asymptomatic inflammatory (NIH-IV) prostatitis in Chinese men. PLoS One. 2013 Aug 13;8(8):e71298. doi: 10.1371/journal.pone.0071298. PMID: 23967188; PMCID: PMC3742742.
https://pubmed.ncbi.nlm.nih.gov/23967188/
43. Porta C, Larghi P, Rimoldi M, Totaro MG, Allavena P, Mantovani A, Sica A. Cellular and molecular pathways linking inflammation and cancer. Immunobiology. 2009;214(9-10):761-77. doi: 10.1016/j.imbio.2009.06.014. Epub 2009 Jul 17. PMID: 19616341.
https://pubmed.ncbi.nlm.nih.gov/19616341/
44. Del Prete A, Allavena P, Santoro G, Fumarulo R, Corsi MM, Mantovani A. Molecular pathways in cancer-related inflammation. Biochem Med (Zagreb). 2011;21(3):264-75. doi: 10.11613/bm.2011.036. PMID: 22420240.
https://pubmed.ncbi.nlm.nih.gov/22420240/
45. Zappavigna S, Cossu AM, Grimaldi A, Bocchetti M, Ferraro GA, Nicoletti GF, Filosa R, Caraglia M. Anti-Inflammatory Drugs as Anticancer Agents. Int J Mol Sci. 2020 Apr 9;21(7):2605. doi: 10.3390/ijms21072605. PMID: 32283655; PMCID: PMC7177823.
https://pubmed.ncbi.nlm.nih.gov/32283655/
46. Young LS, Rickinson AB. Epstein-Barr virus: 40 years on. Nat Rev Cancer. 2004 Oct;4(10):757-68. doi: 10.1038/nrc1452. PMID: 15510157.
https://pubmed.ncbi.nlm.nih.gov/15510157/
47. Disanto G, Pakpoor J, Morahan JM, Hall C, Meier UC, Giovannoni G, Ramagopalan SV. Epstein-Barr virus, latitude and multiple sclerosis. Mult Scler. 2013 Mar;19(3):362-5. doi: 10.1177/1352458512451942. Epub 2012 Jul 5. PMID: 22767435.
https://pubmed.ncbi.nlm.nih.gov/22767435/
48. Esau D. Viral Causes of Lymphoma: The History of Epstein-Barr Virus and Human T-Lymphotropic Virus 1. Virology (Auckl). 2017 Sep 25;8:1178122X17731772. doi: 10.1177/1178122X17731772. PMID: 28983187; PMCID: PMC5621661.
https://pubmed.ncbi.nlm.nih.gov/28983187/
49. Mui UN, Haley CT, Vangipuram R, Tyring SK. Human oncoviruses: Mucocutaneous manifestations, pathogenesis, therapeutics, and prevention: Hepatitis viruses, human T-cell leukemia viruses, herpesviruses, and Epstein-Barr virus. J Am Acad Dermatol. 2019 Jul;81(1):23-41. doi: 10.1016/j.jaad.2018.10.072. Epub 2018 Nov 29. PMID: 30502415.
https://pubmed.ncbi.nlm.nih.gov/30502415/
50. Ruiz-Pablos M, Paiva B, Montero-Mateo R, Garcia N, Zabaleta A. Epstein-Barr Virus and the Origin of Myalgic Encephalomyelitis or Chronic Fatigue Syndrome. Front Immunol. 2021 Nov 15;12:656797. doi: 10.3389/fimmu.2021.656797. PMID: 34867935; PMCID: PMC8634673.
https://pubmed.ncbi.nlm.nih.gov/34867935/
51. Hibino S, Kawazoe T, Kasahara H, Itoh S, Ishimoto T, Sakata-Yanagimoto M, Taniguchi K. Inflammation-Induced Tumorigenesis and Metastasis. Int J Mol Sci. 2021 May 21;22(11):5421. doi: 10.3390/ijms22115421. PMID: 34063828; PMCID: PMC8196678.
https://pubmed.ncbi.nlm.nih.gov/34063828/
52. Rogers J. The inflammatory response in Alzheimer's disease. J Periodontol. 2008 Aug;79(8 Suppl):1535-43. doi: 10.1902/jop.2008.080171. PMID: 18673008.
https://pubmed.ncbi.nlm.nih.gov/18673008/
53. Lewis, M. D. (2017). Use of Omega-3s in Traumatic Brain Injury. Clin Surg. 2017; 2, 1449.
https://www.clinicsinsurgery.com/open-access/use-of-omega-3s-in-traumati...
54. Laforge M, Elbim C, Frère C, Hémadi M, Massaad C, Nuss P, Benoliel JJ, Becker C. Tissue damage from neutrophil-induced oxidative stress in COVID-19. Nat Rev Immunol. 2020 Sep;20(9):515-516. doi: 10.1038/s41577-020-0407-1. Erratum in: Nat Rev Immunol. 2020 Aug 10;: PMID: 32728221; PMCID: PMC7388427.
https://pubmed.ncbi.nlm.nih.gov/32728221/
55. Mazumdar A, Adak S, Chatterjee R, Banerjee RK. Mechanism-based inactivation of lacrimal-gland peroxidase by phenylhydrazine: a suicidal substrate to probe the active site. Biochem J. 1997 Jun 15;324 ( Pt 3)(Pt 3):713-9. doi: 10.1042/bj3240713. PMID: 9210393; PMCID: PMC1218485.
https://pubmed.ncbi.nlm.nih.gov/9210393/
56. Derscheid RJ, van Geelen A, Berkebile AR, Gallup JM, Hostetter SJ, Banfi B, McCray PB Jr, Ackermann MR. Increased concentration of iodide in airway secretions is associated with reduced respiratory syncytial virus disease severity. Am J Respir Cell Mol Biol. 2014 Feb;50(2):389-97. doi: 10.1165/rcmb.2012-0529OC. PMID: 24053146; PMCID: PMC3930944.
https://pubmed.ncbi.nlm.nih.gov/24053146/
57. Aydogan F, Ayhan Tuzcu E, Aydogan A, Akkucuk S, Coskun M, Ustun I, Gökçe C. Effect of radioactive iodine therapy on lacrimal gland functions in patients with hyperthyroidism. Clin Nucl Med. 2014 Apr;39(4):315-8. doi: 10.1097/RLU.0000000000000308. PMID: 24300361.
https://pubmed.ncbi.nlm.nih.gov/24300361/
58. Smith ML, Sharma S, Singh TP. Iodide supplementation of the anti-viral duox-lactoperoxidase activity may prevent some SARS-CoV-2 infections. Eur J Clin Nutr. 2022 Apr;76(4):629-630. doi: 10.1038/s41430-021-00995-2. Epub 2021 Sep 1. PMID: 34471253; PMCID: PMC8408568.
https://pubmed.ncbi.nlm.nih.gov/34471253/
59. Akiba Y, Leung AM, Bashir MT, Ebrahimi R, Currier JW, Neverova N, Kaunitz JD. Excess iodine exposure acutely increases salivary iodide and antimicrobial hypoiodous acid concentrations in humans. Sci Rep. 2022 Dec 3;12(1):20935. doi: 10.1038/s41598-022-23803-8. PMID: 36463312; PMCID: PMC9719529.
https://pubmed.ncbi.nlm.nih.gov/36463312/
60. Salmin VV, Morgun AV, Olovyannikova RY, Kutyakov VA, Lychkovskaya EV, Brusina EB, Salmina AB. Atmospheric Reactive Oxygen Species and Some Aspects of the Antiviral Protection at the Respiratory Epithelium. Biochem Mosc Suppl B Biomed Chem. 2022;16(2):79-90. doi: 10.1134/S1990750822020068. Epub 2022 May 17. PMID: 35601461; PMCID: PMC9113385.
https://pubmed.ncbi.nlm.nih.gov/35601461/
61. Zhang H, Qin L. Positive feedback loop between dietary nitrate intake and oral health. Nutr Res. 2023 Jul;115:1-12. doi: 10.1016/j.nutres.2023.04.008. Epub 2023 Apr 29. PMID: 37207592
https://pubmed.ncbi.nlm.nih.gov/37207592/
62. Tang YM, Wang DG, Li J, Li XH, Wang Q, Liu N, Liu WT, Li YX. Relationships between micronutrient losses in sweat and blood pressure among heat-exposed steelworkers. Ind Health. 2016 Jun 10;54(3):215-23. doi: 10.2486/indhealth.2014-0225. Epub 2016 Apr 16. PMID: 27087421; PMCID: PMC4939859.
https://pubmed.ncbi.nlm.nih.gov/27087421/
63. Wang L, Pan L, Han X, Ha MN, Li K, Yu H, Zhang Q, Li Y, Hou C, Wang H. A portable ascorbic acid in sweat analysis system based on highly crystalline conductive nickel-based metal-organic framework (Ni-MOF). J Colloid Interface Sci. 2022 Jun 15;616:326-337. doi: 10.1016/j.jcis.2022.02.058. Epub 2022 Feb 16. PMID: 35219198.
https://pubmed.ncbi.nlm.nih.gov/35219198/
64. Weller R, Pattullo S, Smith L, Golden M, Ormerod A, Benjamin N. Nitric oxide is generated on the skin surface by reduction of sweat nitrate. J Invest Dermatol. 1996 Sep;107(3):327-31. doi: 10.1111/1523-1747.ep12363167. PMID: 8751965.
https://pubmed.ncbi.nlm.nih.gov/8751965/
65. Herb M, Schramm M. Functions of ROS in Macrophages and Antimicrobial Immunity. Antioxidants (Basel). 2021 Feb 19;10(2):313. doi: 10.3390/antiox10020313. PMID: 33669824; PMCID: PMC7923022.
https://pubmed.ncbi.nlm.nih.gov/33669824/
66. Thomas DC. The phagocyte respiratory burst: Historical perspectives and recent advances. Immunol Lett. 2017 Dec;192:88-96. doi: 10.1016/j.imlet.2017.08.016. Epub 2017 Aug 31. PMID: 28864335.
https://pubmed.ncbi.nlm.nih.gov/28864335/
67. Respiratory burst. Wikipedia, accessed 09 April 2024
https://en.wikipedia.org/wiki/Respiratory_burst
68. Muskiet FAJ. Je hebt ze niet nodig en ze kunnen nog schadelijk zijn ook. Supplementen deel 1. Voedingsgeneeskunde 2024;25(1)34-41
https://www.voedingsgeneeskunde.nl/vg-25-1/hebt-nodig-kunnen-nog-schadel...
69. Kaźmierczak-Barańska J, Boguszewska K, Adamus-Grabicka A, Karwowski BT. Two Faces of Vitamin C-Antioxidative and Pro-Oxidative Agent. Nutrients. 2020 May 21;12(5):1501. doi: 10.3390/nu12051501. PMID: 32455696; PMCID: PMC7285147.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7285147/
70. Levine M, Padayatty SJ, Espey MG. Vitamin C: a concentration-function approach yields pharmacology and therapeutic discoveries. Adv Nutr. 2011 Mar;2(2):78-88. doi: 10.3945/an.110.000109. Epub 2011 Mar 10. PMID: 22332036; PMCID: PMC3065766.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3065766/50. Padayatty SJ, Levine M. Vitamin C: the known and the unknown and Goldilocks. Oral Dis. 2016 Sep;22(6):463-93. doi: 10.1111/odi.12446. Epub 2016 Apr 14. PMID: 26808119; PMCID: PMC4959991.
https://pubmed.ncbi.nlm.nih.gov/26808119/
71. Yamasaki H, Imai H, Tanaka A, Otaki JM. Pleiotropic Functions of Nitric Oxide Produced by Ascorbate for the Prevention and Mitigation of COVID-19: A Revaluation of Pauling's Vitamin C Therapy. Microorganisms. 2023 Feb 3;11(2):397. doi: 10.3390/microorganisms11020397. PMID: 36838362; PMCID: PMC9963342.
https://pubmed.ncbi.nlm.nih.gov/36838362/
72. Zhang H, Qin L. Positive feedback loop between dietary nitrate intake and oral health. Nutr Res. 2023 Jul;115:1-12. doi: 10.1016/j.nutres.2023.04.008. Epub 2023 Apr 29. PMID: 37207592
https://pubmed.ncbi.nlm.nih.gov/37207592/
73. Hickling DR, Nitti VW. Management of recurrent urinary tract infections in healthy adult women. Rev Urol. 2013;15(2):41-8. PMID: 24082842; PMCID: PMC3784967.
https://pubmed.ncbi.nlm.nih.gov/24082842/
73a. Banerjee S, Hawksby C, Miller S, Dahill S, Beattie AD, McColl KE. Effect of Helicobacter pylori and its eradication on gastric juice ascorbic acid. Gut. 1994 Mar;35(3):317-22. doi: 10.1136/gut.35.3.317. PMID: 8150339; PMCID: PMC1374582.
https://pubmed.ncbi.nlm.nih.gov/8150339/
73b. Zhang ZW, Patchett SE, Perrett D, Katelaris PH, Domizio P, Farthing MJ. The relation between gastric vitamin C concentrations, mucosal histology, and CagA seropositivity in the human stomach. Gut. 1998 Sep;43(3):322-6. doi: 10.1136/gut.43.3.322. PMID: 9863475; PMCID: PMC1727232.
https://pubmed.ncbi.nlm.nih.gov/9863475/
74. RADAR in coproductie met het Voedingscentrum. Vitaminepillen, potje onzin of toch niet?, Accessed 30-12-2023
https://radarplus.nl/vitaminepillen-potje-onzin-of-toch-niet/
75. Institute of Medicine (US) Panel on Dietary Antioxidants and Related Compounds. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. Washington (DC): National Academies Press (US); 2000.
https://www.ncbi.nlm.nih.gov/books/NBK225483/pdf/Bookshelf_NBK225483.pdf
76. Carr AC, Lykkesfeldt J. Discrepancies in global vitamin C recommendations: a review of RDA criteria and underlying health perspectives. Crit Rev Food Sci Nutr. 2021;61(5):742-755. doi: 10.1080/10408398.2020.1744513. Epub 2020 Mar 30. PMID: 32223303.
https://pubmed.ncbi.nlm.nih.gov/32223303/
77. King, G., Beins, M., Larkin, J., Summers, B., & Ordman, A. B. (1994). Rate of excretion of vitamin C in human urine. Age, 17, 87-92.
https://link.springer.com/article/10.1007/BF02435011
78. Lindblad M, Tveden-Nyborg P, Lykkesfeldt J. Regulation of vitamin C homeostasis during deficiency. Nutrients. 2013 Jul 25;5(8):2860-79. doi: 10.3390/nu5082860. PMID: 23892714; PMCID: PMC3775232.
https://pubmed.ncbi.nlm.nih.gov/23892714/
78a. Lee, W. J. (2019). Vitamin c in human health and disease: Effects, mechanisms of action, and new guidance on intake. Springer.
https://link.springer.com/book/10.1007/978-94-024-1713-5
78b. Milton K. Micronutrient intakes of wild primates: are humans different? Comp Biochem Physiol A Mol Integr Physiol. 2003 Sep;136(1):47-59. doi: 10.1016/s1095-6433(03)00084-9. PMID: 14527629.
https://pubmed.ncbi.nlm.nih.gov/14527629/
79. Matés JM, Pérez-Gómez C, Núñez de Castro I. Antioxidant enzymes and human diseases. Clin Biochem. 1999 Nov;32(8):595-603. doi: 10.1016/s0009-9120(99)00075-2. PMID: 10638941.
https://pubmed.ncbi.nlm.nih.gov/10638941/
80. Stoutjesdijk E, Schaafsma A, Dijck-Brouwer DAJ, Muskiet FAJ. Iodine status during pregnancy and lactation: a pilot study in the Netherlands. Neth J Med. 2018 Jul;76(5):210-217. PMID: 30019676.
https://pubmed.ncbi.nlm.nih.gov/30019676/
81. Mayunga KC, Lim-A-Po M, Lubberts J, Stoutjesdijk E, Touw DJ, Muskiet FAJ, Dijck-Brouwer DAJ. Pregnant Dutch Women Have Inadequate Iodine Status and Selenium Intake. Nutrients. 2022 Sep 22;14(19):3936. doi: 10.3390/nu14193936. PMID: 36235589; PMCID: PMC9572179.
https://pubmed.ncbi.nlm.nih.gov/36235589/
82. Muskiet FAJ, Schaafsma G, Dijck-Brouwer DAJ. Nederland is nu ook officieel seleniumdeficiënt. Voedingsgeneeskunde 2023;24(6)70-71
https://www.voedingsgeneeskunde.nl/vg-24-6/nederland-nu-ook-officieel-se...
83. Verkaik-Kloosterman, J., van Rossum, C., Beukers, M., & Buurma-Rethans, E. (2018). The habitual micronutrient intake of Dutch adults (VCP 2007-2010) compared with dietary reference values set by the Health Council of the Netherlands (2014) and EFSA (2010-2017).
https://www.rivm.nl/sites/default/files/2018-11/Memo_habitualmicronutint...
84. Kaczor, T. (2014). Iodine and cancer a summary of the evidence to date. Nat Med J, 6(6), 2014-06.
https://www.naturalmedicinejournal.com/journal/iodine-and-cancer
85. Schrauzer GN, White DA, Schneider CJ. Cancer mortality correlation studies--III: statistical associations with dietary selenium intakes. Bioinorg Chem. 1977;7(1):23-31. doi: 10.1016/s0006-3061(00)80126-x. PMID: 856291.
https://pubmed.ncbi.nlm.nih.gov/856291/
86. Shimizu H, Ross RK, Bernstein L, Yatani R, Henderson BE, Mack TM. Cancers of the prostate and breast among Japanese and white immigrants in Los Angeles County. Br J Cancer. 1991 Jun;63(6):963-6. doi: 10.1038/bjc.1991.210. PMID: 2069852; PMCID: PMC1972548.
https://pubmed.ncbi.nlm.nih.gov/2069852/
87. Koletzko B, Boey CC, Campoy C, Carlson SE, Chang N, Guillermo-Tuazon MA, Joshi S, Prell C, Quak SH, Sjarif DR, Su Y, Supapannachart S, Yamashiro Y, Osendarp SJ. Current information and Asian perspectives on long-chain polyunsaturated fatty acids in pregnancy, lactation, and infancy: systematic review and practice recommendations from an early nutrition academy workshop. Ann Nutr Metab. 2014;65(1):49-80. doi: 10.1159/000365767. Epub 2014 Sep 16. PMID: 25227906.
https://pubmed.ncbi.nlm.nih.gov/25227906/
88. Hallberg, Ö., Huttunen, P., & Johansson, O. (2014). Cancer incidence vs. population average sleep duration on spring mattresses. Adv. Stud. Med. Sci, 2, 17-30.
https://electromagnetichealth.org/wp-content/uploads/2015/01/Hallberg_et...
89. Kimura T, Egawa S. Epidemiology of prostate cancer in Asian countries. Int J Urol. 2018 Jun;25(6):524-531. doi: 10.1111/iju.13593. Epub 2018 May 8. PMID: 29740894.
https://pubmed.ncbi.nlm.nih.gov/29740894/
90. Miller, D. W. (2006). Extrathyroidal benefits of iodine. Journal of American Physicians and Surgeons, 11(4), 106.
https://excellentsource.com/images/stories/references/pdfs/Extra%20thyro...
91. Oster O, Schmiedel G, Prellwitz W. The organ distribution of selenium in German adults. Biol Trace Elem Res. 1988 Jan-Apr;15:23-45. doi: 10.1007/BF02990125. PMID: 2484520.
https://pubmed.ncbi.nlm.nih.gov/2484520/
92. Zhou BF, Stamler J, Dennis B, Moag-Stahlberg A, Okuda N, Robertson C, Zhao L, Chan Q, Elliott P; INTERMAP Research Group. Nutrient intakes of middle-aged men and women in China, Japan, United Kingdom, and United States in the late 1990s: the INTERMAP study. J Hum Hypertens. 2003 Sep;17(9):623-30. doi: 10.1038/sj.jhh.1001605. PMID: 13679952; PMCID: PMC6561109.
https://pubmed.ncbi.nlm.nih.gov/13679952/
93. Zava TT, Zava DT. Assessment of Japanese iodine intake based on seaweed consumption in Japan: A literature-based analysis. Thyroid Res. 2011 Oct 5;4:14. doi: 10.1186/1756-6614-4-14. PMID: 21975053; PMCID: PMC3204293.
https://pubmed.ncbi.nlm.nih.gov/21975053/
94. Fuse Y, Ito Y, Shishiba Y, Irie M. Current Iodine Status in Japan: A Cross-sectional Nationwide Survey of Schoolchildren, 2014-2019. J Clin Endocrinol Metab. 2022 Apr 19;107(5):e2065-e2079. doi: 10.1210/clinem/dgab919. PMID: 34935958.
https://pubmed.ncbi.nlm.nih.gov/34935958/
95. Institute of Medicine (US) Panel on Micronutrients. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc; The National Academic Press: Washington, DC, USA, 2001.
https://pubmed.ncbi.nlm.nih.gov/25057538/
96. Overview on Tolerable Upper Intake Levels as derived by the Scientific Committee on Food (SCF) and the EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA)
https://www.efsa.europa.eu/sites/default/files/assets/UL_Summary_tables.pdf
97. Noahsen P, Kleist I, Larsen HM, Andersen S. Intake of seaweed as part of a single sushi meal, iodine excretion and thyroid function in euthyroid subjects: a randomized dinner study. J Endocrinol Invest. 2020 Apr;43(4):431-438. doi: 10.1007/s40618-019-01122-6. Epub 2019 Sep 30. PMID: 31571150.
https://pubmed.ncbi.nlm.nih.gov/31571150/
98. Jin YJ, Kwon MJ, Kim JH, Kim JH, Choi HG. Association between Thyroid Cancer and Breast Cancer: Two Longitudinal Follow-Up Studies Using a National Health Screening Cohort. J Pers Med. 2022 Jan 20;12(2):133. doi: 10.3390/jpm12020133. PMID: 35207622; PMCID: PMC8880453.
https://pubmed.ncbi.nlm.nih.gov/35207622/
99. Manjer J, Sandsveden M, Borgquist S. Serum Iodine and Breast Cancer Risk: A Prospective Nested Case-Control Study Stratified for Selenium Levels. Cancer Epidemiol Biomarkers Prev. 2020 Jul;29(7):1335-1340. doi: 10.1158/1055-9965.EPI-20-0122. Epub 2020 May 26. PMID: 32457181.
https://pubmed.ncbi.nlm.nih.gov/32457181/
100. Szwiec M, Marciniak W, Derkacz R, Huzarski T, Gronwald J, Cybulski C, Dębniak T, Jakubowska A, Lener M, Falco M, Kładny J, Baszuk P, Duszyński J, Kotsopoulos J, Narod SA, Lubiński J. Serum Selenium Level Predicts 10-Year Survival after Breast Cancer. Nutrients. 2021 Mar 16;13(3):953. doi: 10.3390/nu13030953. PMID: 33809461; PMCID: PMC7998294.
https://pubmed.ncbi.nlm.nih.gov/33809461/
101. Moreno-Vega A, Vega-Riveroll L, Ayala T, Peralta G, Torres-Martel JM, Rojas J, Mondragón P, Domínguez A, De Obaldía R, Avecilla-Guerrero C, Anguiano B, Delgado-González E, Zambrano-Estrada X, Cuenca-Micó O, De La Puente Flores O, Varela-Echavarría A, Aceves C. Adjuvant Effect of Molecular Iodine in Conventional Chemotherapy for Breast Cancer. Randomized Pilot Study. Nutrients. 2019 Jul 17;11(7):1623. doi: 10.3390/nu11071623. PMID: 31319484; PMCID: PMC6682905.
https://pubmed.ncbi.nlm.nih.gov/31319484/
102. Anguiano B, Álvarez L, Delgado-González E, Ortiz-Martínez Z, Montes de Oca C, Morales G, Aceves C. Protective effects of iodine on rat prostate inflammation induced by sex hormones and on the DU145 prostate cancer cell line treated with TNF. Mol Cell Endocrinol. 2023 Jul 15;572:111957. doi: 10.1016/j.mce.2023.111957. Epub 2023 May 14. PMID: 37192707.
https://pubmed.ncbi.nlm.nih.gov/37192707/
103. Aceves C, Anguiano B, Delgado G. The extrathyronine actions of iodine as antioxidant, apoptotic, and differentiation factor in various tissues. Thyroid. 2013 Aug;23(8):938-46. doi: 10.1089/thy.2012.0579. PMID: 23607319; PMCID: PMC3752513.
https://pubmed.ncbi.nlm.nih.gov/23607319/
104. Cavalieri RR. Iodine metabolism and thyroid physiology: current concepts. Thyroid. 1997 Apr;7(2):177-81. doi: 10.1089/thy.1997.7.177. PMID: 9133680.
https://pubmed.ncbi.nlm.nih.gov/9133680/
105. Bai XY, Qu X, Jiang X, Xu Z, Yang Y, Su Q, Wang M, Wu H. Association between Dietary Vitamin C Intake and Risk of Prostate Cancer: A Meta-analysis Involving 103,658 Subjects. J Cancer. 2015 Jul 28;6(9):913-21. doi: 10.7150/jca.12162. PMID: 26284143; PMCID: PMC4532989.
https://pubmed.ncbi.nlm.nih.gov/26284143/
106. Bourdoux P, Delange F, Gerard M, Mafuta M, Hanson A, Ermans AM. Evidence that cassava ingestion increases thiocyanate formation: a possible etiologic factor in endemic goiter. J Clin Endocrinol Metab. 1978 Apr;46(4):613-21. doi: 10.1210/jcem-46-4-613. PMID: 755045.
https://pubmed.ncbi.nlm.nih.gov/755045/
107. Ravera S, Reyna-Neyra A, Ferrandino G, Amzel LM, Carrasco N. The Sodium/Iodide Symporter (NIS): Molecular Physiology and Preclinical and Clinical Applications. Annu Rev Physiol. 2017 Feb 10;79:261-289. doi: 10.1146/annurev-physiol-022516-034125. PMID: 28192058; PMCID: PMC5739519.
https://pubmed.ncbi.nlm.nih.gov/28192058/
108. Calder PC, Carr AC, Gombart AF, Eggersdorfer M. Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections. Nutrients. 2020 Apr 23;12(4):1181. doi: 10.3390/nu12041181. PMID: 32340216; PMCID: PMC7230749.
https://pubmed.ncbi.nlm.nih.gov/32340216/
109. Gombart AF, Pierre A, Maggini S. A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection. Nutrients. 2020 Jan 16;12(1):236. doi: 10.3390/nu12010236. PMID: 31963293; PMCID: PMC7019735.
https://pubmed.ncbi.nlm.nih.gov/31963293/
110. Schomburg L. Selenium Deficiency Due to Diet, Pregnancy, Severe Illness, or COVID-19-A Preventable Trigger for Autoimmune Disease. Int J Mol Sci. 2021 Aug 8;22(16):8532. doi: 10.3390/ijms22168532. PMID: 34445238; PMCID: PMC8395178.
https://pubmed.ncbi.nlm.nih.gov/34445238/
111. Blomhoff, R., Andersen, R., Arnesen, E. K., Christensen, J. J., Eneroth, H., Erkkola, M., ... & Trolle, E. (2023). Nordic Nutrition Recommendations 2023: Integrating Environmental Aspects.
https://www.diva-portal.org/smash/record.jsf?dswid=-4899&pid=diva2%3A176...